This isn’t for everybody. From a February 23, 2023 news item on Nanowerk, Note: A link has been removed,
The boundaries between biology and technology are becoming blurred. Researchers at Linköping, Lund, and Gothenburg universities in Sweden have successfully grown electrodes in living tissue using the body’s molecules as triggers. The result, published in the journal Science (“Metabolite-induced in vivo fabrication of substrate-free organic bioelectronics”), paves the way for the formation of fully integrated electronic circuits in living organisms.
I have two news releases for this research. First, the February 23, 2023 American Association for the Advancement of Science (AAAS) news release on EurekAlert,
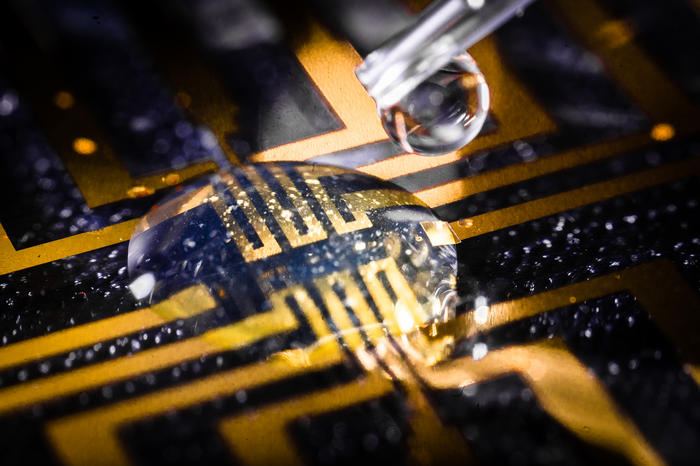
Researchers have developed a way to make bioelectronics directly inside living tissues, an approach they tested by making electrodes in the brain, heart, and fin tissue of living zebrafish, as well as in isolated mammalian muscle tissues. According to the authors, the new method paves the way for in vivo fabrication of fully integrated electronic circuits within the nervous system and other living tissue. “Safety and stability analyses over long periods will be essential to determining whether such technology is useful for chronic implantations,” writes Sahika Inal in a related Perspective. “However, the strategy … suggests that any living tissue can turn into electronic matter and brings the field closer to generating seamless biotic-abiotic interfaces with a potentially long lifetime and minimum harm to tissues.” Implantable electronic devices that can interface with soft biological neural tissues offer a valuable approach to studying the complex electrical signaling of the nervous system and enable the therapeutic modulation of neural circuitry to prevent or treat various diseases and disorders. However, conventional bioelectronic implants often require the use of rigid electronic substrates that are incompatible with delicate living tissues and can provoke injury and inflammation that can affect a device’s electrical properties and long-term performance. Overcoming the incompatibility between static, solid-state electronic materials and dynamic, soft biological tissues has proven challenging. Here, Xenofon Strakosas and colleagues present a method to fabricate polymer-based, substrate-free electronic conducting materials directly inside a tissue. Strakosas et al. developed a complex molecular precursor cocktail that, when injected into a tissue, uses endogenous metabolites (glucose and lactate) to induce polymerization of organic precursors to form conducting polymer gels. To demonstrate the approach, the authors “grew” gel electrodes in the brain, heart, and fin tissue of living zebrafish, with no signs of tissue damage, and in isolated mammalian muscle tissues, including beef, pork and chicken. In medicinal leeches, they showed how the conducting gel could interface nervous tissue with electrodes on a tiny flexible probe.
The second is the February 23, 2023 Linköping University press release on EurekAlert, which originated the news item, and it provides further insight,
“For several decades, we have tried to create electronics that mimic biology. Now we let biology create the electronics for us,” says Professor Magnus Berggren at the Laboratory for Organic Electronics, LOE, at Linköping University.
Linking electronics to biological tissue is important to understand complex biological functions, combat diseases in the brain, and develop future interfaces between man and machine. However, conventional bioelectronics, developed in parallel with the semiconductor industry, have a fixed and static design that is difficult, if not impossible, to combine with living biological signal systems.
To bridge this gap between biology and technology, researchers have developed a method for creating soft, substrate-free, electronically conductive materials in living tissue. By injecting a gel containing enzymes as the “assembly molecules”, the researchers were able to grow electrodes in the tissue of zebrafish and medicinal leeches.
“Contact with the body’s substances changes the structure of the gel and makes it electrically conductive, which it isn’t before injection. Depending on the tissue, we can also adjust the composition of the gel to get the electrical process going,” says Xenofon Strakosas, researcher at LOE and Lund University and one of the study’s main authors.
The body’s endogenous molecules are enough to trigger the formation of electrodes. There is no need for genetic modification or external signals, such as light or electrical energy, which has been necessary in previous experiments. The Swedish researchers are the first in the world to succeed in this.
Their study paves the way for a new paradigm in bioelectronics. Where it previously took implanted physical objects to start electronic processes in the body, injection of a viscous gel will be enough in the future.
In their study, the researchers further show that the method can target the electronically conducting material to specific biological substructures and thereby create suitable interfaces for nerve stimulation. In the long term, the fabrication of fully integrated electronic circuits in living organisms may be possible.
In experiments conducted at Lund University, the team successfully achieved electrode formation in the brain, heart, and tail fins of zebrafish and around the nervous tissue of medicinal leeches. The animals were not harmed by the injected gel and were otherwise not affected by the electrode formation. One of the many challenges in these trials was to take the animals’ immune system into account.
“By making smart changes to the chemistry, we were able to develop electrodes that were accepted by the brain tissue and immune system. The zebrafish is an excellent model for the study of organic electrodes in brains,” says Professor Roger Olsson at the Medical Faculty at Lund University, who also has a chemistry laboratory at the University of Gothenburg.
It was Professor Roger Olsson who took the initiative for the study, after he read about the electronic rose developed by researchers at Linköping University in 2015. One research problem, and an important difference between plants and animals, was the difference in cell structure. Whereas plants have rigid cell walls which allow for the formation of electrodes, animal cells are more like a soft mass. Creating a gel with enough structure and the right combination of substances to form electrodes in such surroundings was a challenge that took many years to solve.
“Our results open up for completely new ways of thinking about biology and electronics. We still have a range of problems to solve, but this study is a good starting point for future research,” says Hanne Biesmans, PhD student at LOE and one of the main authors.
Here’s a link to and a citation for the paper,
Metabolite-induced in vivo fabrication of substrate-free organic bioelectronics by Xenofon Strakosas, Hanne Biesmans, Tobias Abrahamsson, Karin Hellman, Malin Silverå Ejneby, Mary J. Donahue, Peter Ekström, Fredrik Ek, Marios Savvakis, Martin Hjort, David Bliman, Mathieu Linares, Caroline Lindholm, Eleni Stavrinidou, Jennifer Y. Gerasimov, Daniel T. Simon, Roger Olsson, and Magnus Berggren. Science 23 Feb 2023 Vol 379, Issue 6634 pp. 795-802 DOI: 10.1126/science.adc9998
This paper is behind a paywall.