Whoever wrote this Technion-Israel Institute of Technology November 28, 2021 press release (also on EurekAlert) they seem to have had a lot of fun doing it,
“Sutures? That’s practically medieval!”
It is a staple of science fiction to mock sutures as outdated. The technique has, after all, been in use for at least 5,000 years. Surely medicine should have advanced since ancient Egypt. Professor Hossam Haick from the Wolfson Department of Chemical Engineering at the Technion has finally turned science fiction into reality. His lab succeeded in creating a smart sutureless dressing that binds the wound together, wards off infection, and reports on the wound’s condition directly to the doctors’ computers. Their study was published in Advanced Materials.
Current surgical procedures entail the surgeon cutting the human body, doing what needs to be done, and sewing the wound shut – an invasive procedure that damages surrounding healthy tissue. Some sutures degrade by themselves – or should degrade – as the wound heals. Others need to be manually removed. Dressing is then applied over the wound and medical personnel monitor the wound by removing the dressing to allow observation for signs of infection like swelling, redness, and heat. This procedure is painful to the patient, and disruptive to healing, but it is unavoidable. Working with these methods also mean that infection is often discovered late, since it takes time for visible signs to appear, and more time for the inspection to come round and see them. In developed countries, with good sanitation available, about 20% of patients develop infections post-surgery, necessitating additional treatment and extending the time to recovery. The figure and consequences are much worse in developing countries.
How will it work with Prof. Haick’s new dressing?
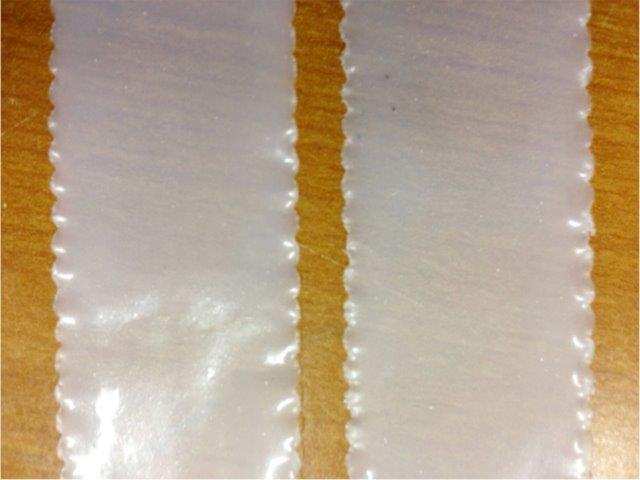
Prior to beginning a procedure, the dressing – which is very much like a smart band-aid – developed by Prof. Haick’s lab will be applied to the site of the planned incision. The incision will then be made through it. Following the surgery, the two ends of the wound will be brought together, and within three seconds the dressing will bind itself together, holding the wound closed, similarly to sutures. From then, the dressing will be continuously monitoring the wound, tracking the healing process, checking for signs of infection like changes in temperature, pH, and glucose levels, and report to the medical personnel’s smartphones or other devices. The dressing will also itself release antibiotics onto the wound area, preventing infection.
“I was watching a movie on futuristic robotics with my kids late one night,” said Prof. Haick, “and I thought, what if we could really make self-repairing sensors?”
Most people discard their late-night cinema-inspired ideas. Not Prof. Haick, who, the very next day after his Eureka moment, was researching and making plans. The first publication about a self-healing sensor came in 2015 (read more about it on the Technion website here). At that time, the sensor needed almost 24 hours to repair itself. By 2020, sensors were healing in under a minute (read about the study by Muhammad Khatib, a student in Prof. Haick’s lab here), but while it had multiple applications, it was not yet biocompatible, that is, not usable in contact with skin and blood. Creating a polymer that would be both biocompatible and self-healing was the next step, and one that was achieved by postdoctoral fellow Dr. Ning Tang.
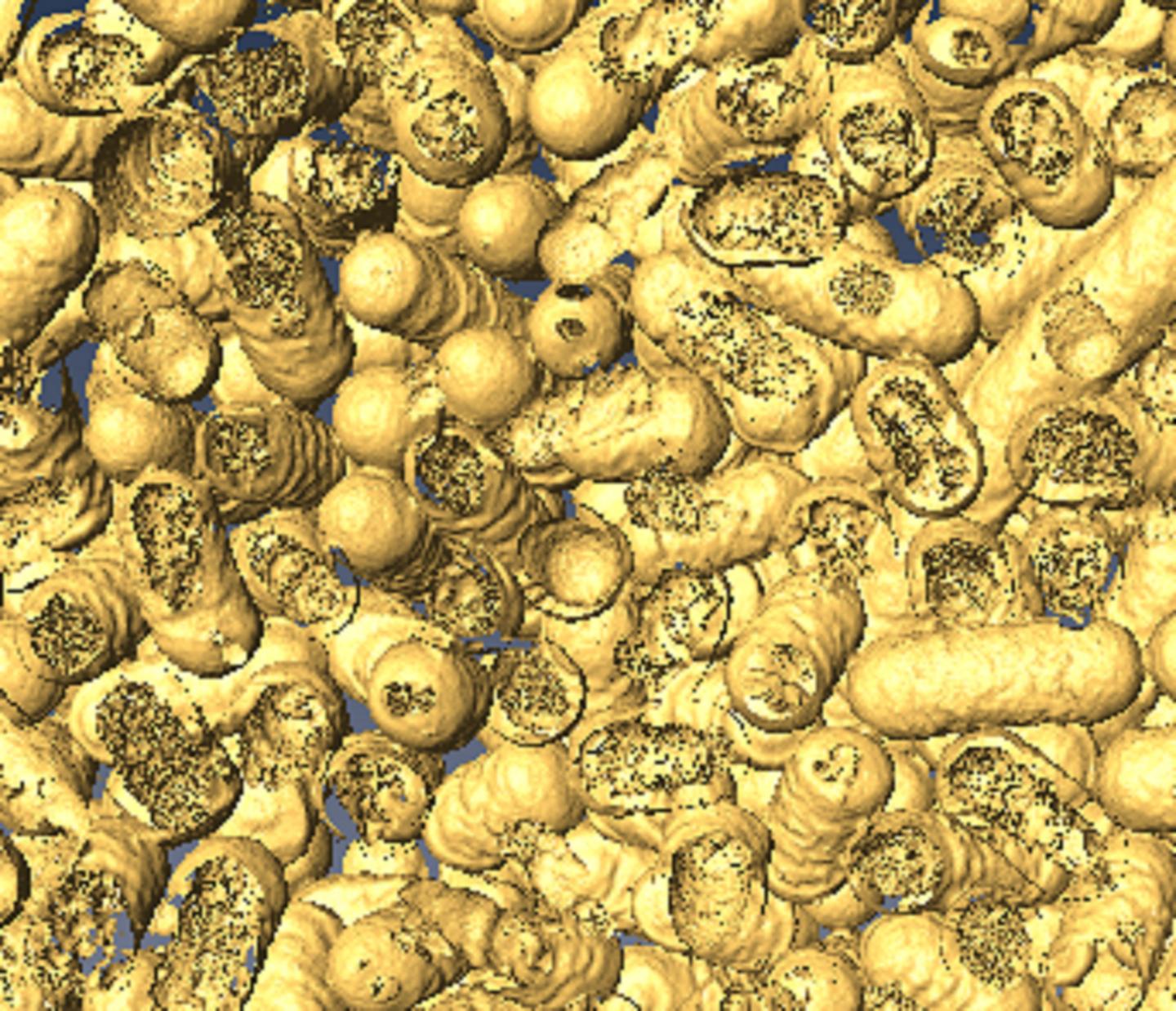
The new polymer is structured like a molecular zipper, made from sulfur and nitrogen: the surgeon’s scalpel opens it; then pressed together, it closes and holds fast. Integrated carbon nanotubes provide electric conductivity and the integration of the sensor array. In experiments, wounds closed with the smart dressing healed as fast as those closed with sutures and showed reduced rates of infection.
“It’s a new approach to wound treatment,” said Prof. Haick. “We introduce the advances of the fourth industrial revolution – smart interconnected devices, into the day-to-day treatment of patients.”
Prof. Haick is the head of the Laboratory for Nanomaterial-based Devices (LNBD) and the Dean of Undergraduate Studies at the Technion. Dr. Ning Tang was a postdoctoral fellow in Prof. Haick’s laboratory and conducted this study as part of his fellowship. He has now been appointed an associate professor in Shanghai Jiao Tong University.
Here’s a link to and a citation for the paper,
Highly Efficient Self-Healing Multifunctional Dressing with Antibacterial Activity for Sutureless Wound Closure and Infected Wound Monitoring by Ning Tang, Rongjun Zhang, Youbin Zheng, Jing Wang, Muhammad Khatib, Xue Jiang, Cheng Zhou, Rawan Omar, Walaa Saliba, Weiwei Wu, Miaomiao Yuan, Daxiang Cui, Hossam Haick. DOI: https://doi.org/10.1002/adma.202106842 First published: 05 November 2021
This paper is behind a paywall.
I usually like to have three links to a news/press release and in my searches for a third source for this press release, I stumbled onto the technioncanada.org website. They seemed to have scooped everyone including Technion as they have a November 25, 2021posting of the press release.