This work on a type of species boundary-crossing could be very disturbing for some folks. That said, here’s more about the science from a July 2, 2021 news item on phys.org,
A year after University at Buffalo [in New York state] scientists demonstrated that it was possible to produce millions of mature human cells in a mouse embryo, they have published a detailed description of the method so that other laboratories can do it, too.
A July 2, 2021 University at Buffalo (UB) news release (also on EurekAlert) by Ellen Goldbaum, which originated the news item, explains why scientists have created these chimeras,
The ability to produce millions of mature human cells in a living organism, called a chimera, which contains the cells of two species, is critical if the ultimate promise of stem cells to treat or cure human disease is to be realized. But to produce those mature cells, human primed stem cells must be converted back into an earlier, less developed naive state so that the human stem cells can co-develop with the inner cell mass in a mouse blastocyst.
The protocol outlining how to do that has now been published in Nature Protocols by the UB scientists. They were invited to publish it because of the significant interest generated by the team’s initial publication describing their breakthrough last May [2020].
“This paper will enable many scientists to use this new platform to study the human disease of their interest,” said Jian Feng, PhD, professor of physiology and biophysics in the Jacobs School of Medicine and Biomedical Sciences at UB and senior author. “Over time, it will transform biomedical research toward a more effective use of the human model system to directly study virtually any inborn condition of an individual. It will stimulate unforeseen discoveries and applications that may fundamentally change our understanding of human biology and medicine.”
The protocol will allow scientists to create animal models that Feng said provide a much more realistic picture of embryonic development than has ever been possible. These more realistic animal models also will have the potential to reveal the mechaniswms behind numerous diseases, especially those that afflict individuals from birth.
Better mouse models
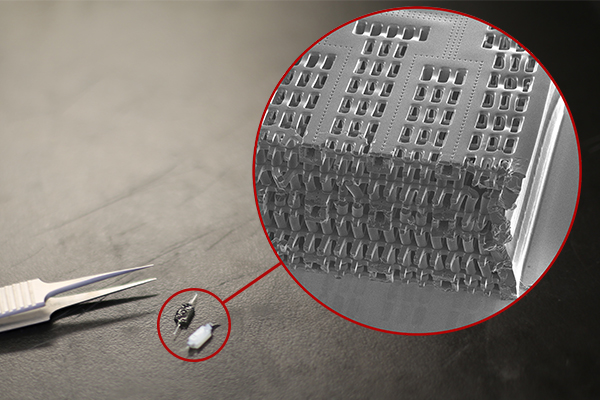
“This step-by-step protocol will benefit the entire field by enabling other scientists to use our methods to generate chimeras to study human diseases that they are experts in,” said Feng. “It will lead to the generation of better mouse models for various human diseases, such as sickle cell anemia, COVID-19 and many others, or various human developmental disorders.” The paper demonstrates how to generate naive human pluripotent stem cells from existing induced pluripotent stem cells that may be derived from patients with various diseases, how to generate mouse-human chimeras using these cells and how to quantify the amount of human cells in the chimeras.
“Using our method, one can now track the development of naive human pluripotent stem cells in mouse-human chimeric embryos in real-time,” said Feng. These stem cells can then be manipulated either genetically or pharmacologically, providing valuable information about human development and disease.
“For example, one can label naive human pluripotent stem cells by inserting green fluorescent protein in a hemoglobin gene to study the development of human red blood cells in mouse-human chimeras,” said Feng.
Another application is to generate humanized mouse models to study many human diseases.
“These mice contain critical human cells, tissues or even organs so that they more accurately reflect the human condition,” said Feng. “With our method, the human cells are made along with the mouse during the development of the mouse embryo. There would be better matching and no rejections, because there are ways for the human cells to be made where there is no competition from their mouse counterparts.”
Organs for transplant in the future
By allowing others to improve and adapt the method to eventually generate chimeras in larger animals, this protocol may also lead to the generation of human organs to address the dire shortage of organs available for transplant, said Feng.
“If naive human pluripotent stem cells are able to generate significant amounts of mature human cells in other larger species, it could be possible to make human tissues or even human organs in chimeric animals,” Feng explained.
This would be possible using blastocyst complementation where, Feng explained, normal pluripotent stem cells from one species can reconstitute an organ for that species in a blastocyst of another species that been genetically modified not to grow that particular organ.
Feng added: “Ultimately, a better understanding of how human cells develop and grow in chimeras may enable the generation of human cells, tissues and organs in a completely artificial system and fundamentally change how we treat many human diseases. Research using chimeras is a bridge that must be crossed to reach that possibility.”
Here’s a link to and a citation for the 2021 article,
Generation of mouse–human chimeric embryos by Boyang Zhang, Hanqin Li, Zhixing Hu, Houbo Jiang, Aimee B. Stablewski, Brandon J. Marzullo, Donald A. Yergeau & Jian Feng. Nature Protocols (2021) DOI: https://doi.org/10.1038/s41596-021-00565-7 Published 02 July 2021
This article is behind a paywall.
Here’s a link to and citation for the 2020 work, which led to the publication of the protocols,
Transient inhibition of mTOR in human pluripotent stem cells enables robust formation of mouse-human chimeric embryos by Zhixing Hu, Hanqin Li, Houbo Jiang, Yong Ren, Xinyang Yu, Jingxin Qiu, Aimee B. Stablewski, Boyang Zhang, Michael J. Buck, Jian Feng. Science Advances 13 May 2020: Vol. 6, no. 20, eaaz0298 DOI: 10.1126/sciadv.aaz0298
This paper is open access.