This first part of this Reading ‘series’, Reading (1 of 2): an artificial intelligence story in British Columbia (Canada) was mostly about how one type of story, in this case,based on a survey, is presented and placed in one or more media outlets. The desired outcome is for more funding by government and for more investors (they tucked in an ad for an upcoming artificial intelligence conference in British Columbia).
This story about zinc-infused underwear for women also uses science to prove its case and it, too, is about raising money. In this case, it’s a Kickstarter campaign to raise money.
If Huha’s (that’s the company name) claims for ‘zinc-infused mineral undies’ are to be believed, the answer is an unequivocal yes. The reality as per the current research on the topic is not quite as conclusive.
The semiotics (symbolism)
Huha features fruit alongside the pictures of their underwear. You’ll see an orange, papaya, and melon in the kickstarter campaign images and on the company website. It seems to be one of those attempts at subliminal communication. Fruit is good for you therefore our underwear is good for you. In fact, our underwear (just like the fruit) has health benefits.
For a deeper dive into the world of semiotics, there’s the ‘be fruitful and multiply’ stricture which is found in more than one religious or cultural orientation and is hard to dismiss once considered.
There is no reason to add fruit to the images other than to suggest benefits from nature and fertility (or fruitfulness). They’re not selling fruit and these ones are not particularly high in zinc. If all you’re looking for is colour, why not vegetables or puppies?
The claims
I don’t have time to review all of the claims but I’ll highlight a few. My biggest problem with the claims is that there are no citations or links to studies, i.e., the research. So, something like this becomes hard to assess,
Most women’s underwear are made with chemical-based, synthetic fibers that lead to yeast and UTI [urinary tract infection] infections, odor, and discomfort. They’ve also been proven to disrupt human hormones, have been linked to cancer, pollute the planet aggressively, and stay in landfills far too long.
There’s more than one path to a UTI and/or odor and/or discomfort but I can see where fabrics that don’t breathe can exacerbate or cause problems of that nature. I have a little more difficulty with the list that follows. I’d like to see the research on underpants disrupting human hormones. Is this strictly a problem for women or could men also be affected? (If you should know, please leave a comment.)
As for ‘linked to cancer’, I’m coming to the conclusion that everything is linked to cancer. Offhand, I’ve been told peanuts, charcoal broiled items (I think it’s the char), and my negative thoughts are all linked to cancer.
One of the last claims in the excerpted section, ‘pollute the planet aggressively’ raises this question.When did underpants become aggressive’?
The final claim seems unexceptional. Our detritus is staying too long in our landfills. Of course, the next question is: how much faster do the Huha underpants degrade in a landfill? That question is not addressed in Kickstarter campaign material.
Talking to someone with more expertise
I contacted Dr. Andrew Maynard, Associate Director at Arizona State University (ASU) School for the Future of Innovation in Society, He has a PhD in physics and longstanding experience in research and evaluation of emerging technologies (for many years he specialized in nanoparticle analysis and aerosol exposure in occupational settings),.
Professor Maynard is a widely recognized expert and public commentator on emerging technologies and their safe and responsible development and use, and has testified before [US] congressional committees on a number of occasions.
None of this makes him infallible but I trust that he always works with integrity and bases his opinions on the best information at hand. I’ve always found him to be a reliable source of information.
Here’s what he had to say (from an October 25, 2019 email),
I suspect that their claims are pushing things too far – from what I can tell, professionals tend to advise against synthetic underwear because of the potential build up of moisture and bacteria and the lack of breathability, and tend to suggest natural materials – which indicating that natural fibers and good practices should be all most people need. I haven’t seen any evidence for an underwear crisis here, and one concern is that the company is manufacturing a problem which they then claim to solve. That said, I can’t see anything totally egregious in what they are doing. And the zinc presence makes sense in that it prevents bacterial growth/activity within the fabric, thus reducing the chances of odor and infection.
Pharmaceutical grade zinc and research into underwear
I was a little curious about ‘pharmaceutical grade’ zinc as my online searches for a description were unsuccessful. Andrew explained that the term likely means ‘high purity’ zinc suitable for use in medications rather than the zinc found in roofing panels.
After the reference to ‘pharmaceutical grade’ zinc there’s a reference to ‘smartcel sensitive Zinc’. Here’s more from the smartcel sensitive webpage,
smartcel™ sensitive is skin friendly thanks to zinc oxide’s soothing and anti-inflammatory capabilities. This is especially useful for people with sensitive skin or skin conditions such as eczema or neurodermitis. Since zinc is a component of skin building enzymes, it operates directly on the skin. An active exchange between the fiber and the skin occurs when the garment is worn.
Zinc oxide also acts as a shield against harmful UVA and UVB radiation [it’s used in sunscreens], which can damage our skin cells. Depending on the percentage of smartcel™ sensitive used in any garment, it can provide up to 50 SPF.
Further to this, zinc oxide possesses strong antibacterial properties, especially against odour causing bacteria, which helps to make garments stay fresh longer. *
I couldn’t see how zinc helps the pH balance in anyone’s vagina as claimed in the Kickstarter campaign and smartcel, on its ‘sensitive’ webpage, doesn’t make that claim but I found an answer in an April 4, 2017 Q&A (question and answer) interview by Jocelyn Cavallo for Medium,
What women need to know about their vaginal p
Q & A with Dr. Joanna Ellington
A woman’s vagina is a pretty amazing body part. Not only can it be a source of pleasure but it also can help create and bring new life into the world. On top of all that, it has the extraordinary ability to keep itself clean by secreting natural fluids and maintaining a healthy pH to encourage the growth of good bacteria and discourage harmful bacteria from moving in. Despite being so important, many women are never taught the vital role that pH plays in their vaginal health or how to keep it in balance.
We recently interviewed renowned Reproductive Physiologist and inventor of IsoFresh Balancing Vaginal Gel, Dr. Joanna Ellington, to give us the low down on what every woman needs to know about their vaginal pH and how to maintain a healthy level.
What is pH?
Dr. Ellington: PH is a scale of acidity and alkalinity. The measurements range from 0 to 14: a pH lower than 7 is acidic and a pH higher than 7 is considered alkaline.
What is the “perfect” pH level for a woman’s vagina?
Dr. E.: For most women of a reproductive age vaginal pH should be 4.5 or less. For post-menopausal women this can go up to about 5. The vagina will naturally be at a high pH right after sex, during your period, after you have a baby or during ovulation (your fertile time).
Are there diet and environmental factors that affect a women’s vaginal pH level?
Dr. E.: Yes, iron zinc and manganese have been found to be critical for lactobacillus (healthy bacteria) to function. Many women don’t eat well and should supplement these, especially if they are vegetarian. Additionally, many vegetarians have low estrogen because they do not eat the animal fats that help make our sex steroids. Without estrogen, vaginal pH and bacterial imbalance can occur. It is important that women on these diets ensure good fat intake from other sources, and have estrogen and testosterone and iron levels checked each year.
Do clothing and underwear affect vaginal pH?
Dr. E.: Yes, tight clothing and thong underwear [emphasis mine] have been shown in studies to decrease populations of healthy vaginal bacteria and cause pH changes in the vagina. Even if you wear these sometimes, it is important for your vaginal ecosystem that loose clothing or skirts be worn some too.
…
Yes, Dr. Ellington has the IsoFresh Balancing Vaginal Gel and whether that’s a good product should be researched but all of the information in the excerpt accords with what I’ve heard over the years and fits in nicely with what Andrew said, zinc in underwear could be useful for its antimicrobial properties. Also, note the reference to ‘thong underwear’ as a possible source of difficulty and note that Huha is offering thong and very high cut underwear.
Of course, your underwear may already have zinc in it as this research suggests (thank you, Andrew, for the reference),
Exposure of women to trace elements through the skin by direct contact with underwear clothing by Thao Nguyen & Mahmoud A. Saleh. Journal of Environmental Science and Health, Part A Toxic/Hazardous Substances and Environmental Engineering Volume 52, 2017 – Issue 1 Pages 1-6 DOI: https://doi.org/10.1080/10934529.2016.1221212 Published online: 09 Sep 2016
This paper is behind a paywall but I have access through a membership in the Canadian Academy of Independent Scholars. So, here’s the part I found interesting,
… The main chemical pollutants present in textiles are dyes containing carcinogenic amines, metals, pentachlorophenol, chlorine bleaching, halogen carriers, free formaldehyde, biocides, fire retardants and softeners.[1] Metals are also found in textile products and clothing are used for many purposes: Co [cobalt], Cu [copper], Cr [chromium] and Pb [lead] are used as metal complex dyes, Cr as pigments mordant, Sn as catalyst in synthetic fabrics and as synergists of flame retardants,Ag [silver] as antimicrobials and Ti [titanium] and Zn [zinc] as water repellents and odor preventive agents.[2–5] When present in textile materials, the toxic elements mentioned above represent not only a major environmental problem in the textile industry but also they may impose potential danger to human health by absorption through the skin.[6,7] [emphasis mine] Chronic exposure to low levels of toxic elements has been associated with a number of adverse human health effects.[8–11] Also exposure to high concentration of elements which are considered as essential for humans such as Cu, Co, Fe [iron], Mn [manganese] or Zn among others, can also be harmful.[12] [emphasis mine] Co, Cr, Cu and Ni [nitrogen] are skin sensitizers,[13,14] which may lead to contact dermatitis, also Cr can lead to liver damage, pulmonary congestion and cancer.[15] [emphasis mine] The purpose of the present study was to determine the concentrations of a number of elements in various skin-contact clothes. For risk estimations, the determination of the extractable amounts of heavy metals is of importance, since they reflect their possible impact on human health. [p. 2 PDF]
So, there’s the link to cancer. Maybe.
Are zinc-infused undies a good idea?
It could go either way. (For specifics about the conclusions reached in the study, scroll down to the Ooops! subheading.) I like the idea of using sustainable Eucalyptus-based material (TencelL) for the underwear as I have heard that cotton isn’t sustainably cultivated. As for claims regarding the product’s environmental friendliness, it’s based on wood, specifically, cellulose, which Canadian researchers have been experimenting with at the nanoscale* and they certainly have been touting nanocellulose as environmentally friendly. Tencel’s sustainability page lists a number of environmental certifications from the European Union, Belgium, and the US.
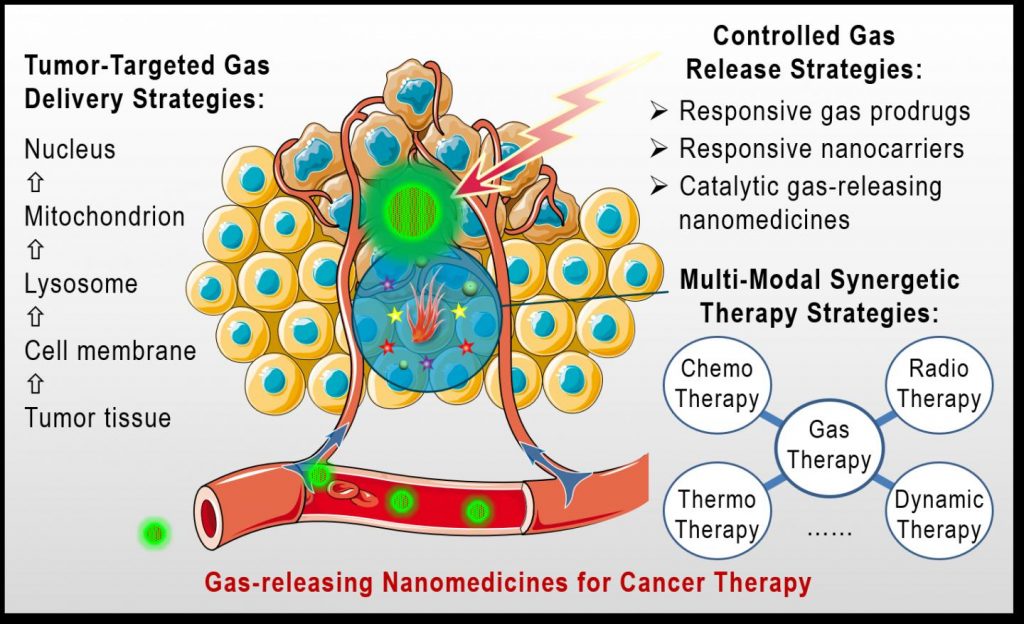
*Somewhere in the Kickstarter campaign material, there’s a reference to nanofibrils and I’m guessing those nanofibrils are Tencel’s wood fibers at the nanoscale. As well, I’m guessing that smartcel’s fabric contains zinc oxide nanoparticles.
Whether or not you need more zinc is something you need to determine for yourself. Finding out if the pH balance in your vagina is within a healthy range might be a good way to start. It would also be nice to know how much zinc is in the underwear and whether it’s being used antimicrobial properties and/or as a source for one of minerals necessary for your health.
How the Kickstarter campaign is going
At the time of this posting, they’ve reached a little over $24,000 with six days left. The goal was $10,000. Sadly, there are no questions in the FAQ (frequently asked questions).
Reading tips
It’s exhausting trying to track down authenticity. In this case, there were health and environmental claims but I do have a few suggestions.
- Look at the imagery critically and try to ignore the hyperbole.
- How specific are the claims? e.g., How much zinc is there in the underpants?
- Who are their experts and how trustworthy are the agencies/companies mentioned?
- If research is cited, are the publishers reputable and is the journal reputable?
- Does it make sense given your own experience?
- What are the consequences if you make a mistake?
Overblown claims and vague intimations of disease are not usually good signs. Conversely, someone with great credential may not be trustworthy which is why I usually try to find more than one source for confirmation. The person behind this campaign and the Huha company is Alexa Suter. She’s based in Vancouver, Canada and seems to have spent most of her time as a writer and social media and video producer with a few forays into sales and real estate. I wonder if she’s modeling herself and her current lifestyle entrepreneurial effort on Gwyneth Paltrow and her lifestyle company, Goop.
Huha underwear may fulfill its claims or it may be just another pair of underwear or it may be unhealthy. As for the environmentally friendly claims, let’s hope that the case. On a personal level, I’m more hopeful about that.
Regardless, the underwear is not cheap. The smallest pledge that will get your underwear (a three-pack) is $65 CAD.
Ooops! ETA: November 8, 2019:
I forgot to include the conclusion the researchers arrived at and some details on how they arrived at those conclusions. First, they tested 120 pairs of underpants in all sorts of colours and made in different parts of the world.
Second, some underpants showed excessive levels of metals. Cotton was the most likely material to show excess although nylon and polyester can also be problematic. To put this into proportion and with reference to zinc, “Zn exceeded the limit in 4% of the tested samples
and was found mostly in samples manufactured in China.” [p. 6 PDF] Finally, dark colours tested for higher levels of metals than light colours.
While it doesn’t mention underpants as such, there’s a November 8, 2019 article ‘Five things everyone with a vagina should know‘ by Paula McGrath for BBC news online. McGrath’s health expert is Dr. Jen Gunter, a physician whose specialties are obstetrics, gynaecology, and pain.