This story got me to thinking about what happens when any kind of implant company (pacemaker, deep brain stimulator, etc.) goes bankrupt or is acquired by another company with a different business model.
As I worked on this piece, more issues were raised and the scope expanded to include prosthetics along with implants while the focus narrowed to neuro as in, neural implants and neuroprosthetics. At the same time, I found salient examples for this posting in other medical advances such as gene editing.
In sum, all references to implants and prosthetics are to neural devices and some issues are illustrated with salient examples from other medical advances (specifically, gene editing).
Definitions (for those who find them useful)
The US Food and Drug Administration defines implants and prosthetics,
Medical implants are devices or tissues that are placed inside or on the surface of the body. Many implants are prosthetics, intended to replace missing body parts. Other implants deliver medication, monitor body functions, or provide support to organs and tissues.
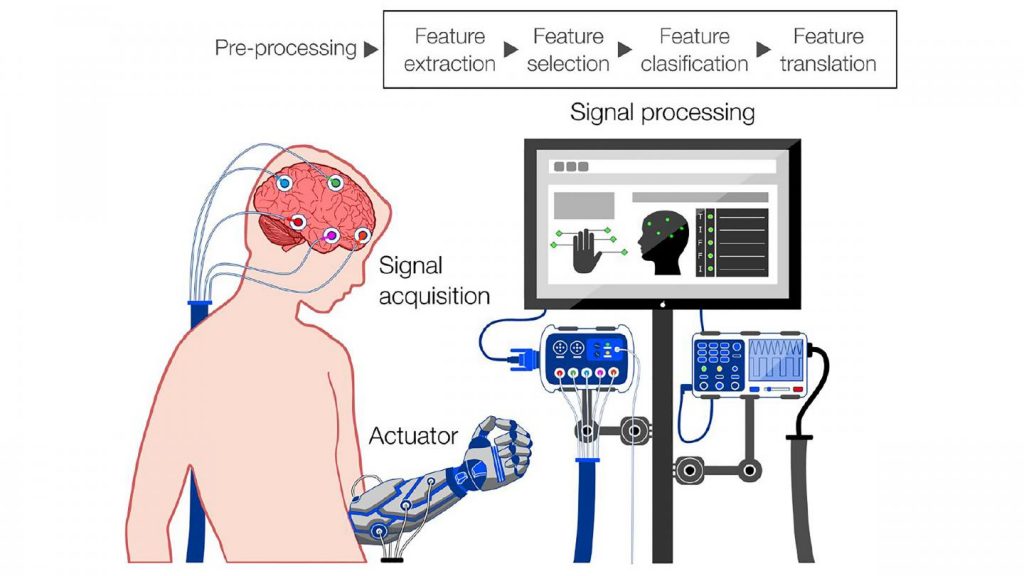
As for what constitutes a neural implant/neuroprosthetic, there’s this from Emily Waltz’s January 20, 2020 article (How Do Neural Implants Work? Neural implants are used for deep brain stimulation, vagus nerve stimulation, and mind-controlled prostheses) for the Institute of Electrical and Electronics Engineers (IEEE) Spectrum magazine,
A neural implant, then, is a device—typically an electrode of some kind—that’s inserted into the body, comes into contact with tissues that contain neurons, and interacts with those neurons in some way.
…
Now, let’s start with the recent near bankruptcy of a retinal implant company.
The company goes bust (more or less)
From a February 25, 2022 Science Friday (a National Public Radio program) posting/audio file, Note: Links have been removed,
Barbara Campbell was walking through a New York City subway station during rush hour when her world abruptly went dark. For four years, Campbell had been using a high-tech implant in her left eye that gave her a crude kind of bionic vision, partially compensating for the genetic disease that had rendered her completely blind in her 30s. “I remember exactly where I was: I was switching from the 6 train to the F train,” Campbell tells IEEE Spectrum. “I was about to go down the stairs, and all of a sudden I heard a little ‘beep, beep, beep’ sound.’”
It wasn’t her phone battery running out. It was her Argus II retinal implant system powering down. The patches of light and dark that she’d been able to see with the implant’s help vanished.
Terry Byland is the only person to have received this kind of implant in both eyes. He got the first-generation Argus I implant, made by the company Second Sight Medical Products, in his right eye in 2004, and the subsequent Argus II implant in his left 11 years later. He helped the company test the technology, spoke to the press movingly about his experiences, and even met Stevie Wonder at a conference. “[I] went from being just a person that was doing the testing to being a spokesman,” he remembers.
Yet in 2020, Byland had to find out secondhand that the company had abandoned the technology and was on the verge of going bankrupt. While his two-implant system is still working, he doesn’t know how long that will be the case. “As long as nothing goes wrong, I’m fine,” he says. “But if something does go wrong with it, well, I’m screwed. Because there’s no way of getting it fixed.”
…
Science Friday and the IEEE [Institute of Electrical and Electronics Engineers] Spectrum magazine collaborated to produce this story. You’ll find the audio files and the transcript of interviews with the authors and one of the implant patients in this February 25, 2022 Science Friday (a National Public Radio program) posting.
Here’s more from the February 15, 2022 IEEE Spectrum article by Eliza Strickland and Mark Harris,
Ross Doerr, another Second Sight patient, doesn’t mince words: “It is fantastic technology and a lousy company,” he says. He received an implant in one eye in 2019 and remembers seeing the shining lights of Christmas trees that holiday season. He was thrilled to learn in early 2020 that he was eligible for software upgrades that could further improve his vision. Yet in the early months of the COVID-19 pandemic, he heard troubling rumors about the company and called his Second Sight vision-rehab therapist. “She said, ‘Well, funny you should call. We all just got laid off,’ ” he remembers. “She said, ‘By the way, you’re not getting your upgrades.’ ”
These three patients, and more than 350 other blind people around the world with Second Sight’s implants in their eyes, find themselves in a world in which the technology that transformed their lives is just another obsolete gadget. One technical hiccup, one broken wire, and they lose their artificial vision, possibly forever. To add injury to insult: A defunct Argus system in the eye could cause medical complications or interfere with procedures such as MRI scans, and it could be painful or expensive to remove.
…
The writers included some information about what happened to the business, from the February 15, 2022 IEEE Spectrum article, Note: Links have been removed,
After Second Sight discontinued its retinal implant in 2019 and nearly went out of business in 2020, a public offering in June 2021 raised US $57.5 million at $5 per share. The company promised to focus on its ongoing clinical trial of a brain implant, called Orion, that also provides artificial vision. But its stock price plunged to around $1.50, and in February 2022, just before this article was published, the company announced a proposed merger with an early-stage biopharmaceutical company called Nano Precision Medical (NPM). None of Second Sight’s executives will be on the leadership team of the new company, which will focus on developing NPM’s novel implant for drug delivery.The company’s current leadership declined to be interviewed for this article but did provide an emailed statement prior to the merger announcement. It said, in part: “We are a recognized global leader in neuromodulation devices for blindness and are committed to developing new technologies to treat the broadest population of sight-impaired individuals.”
…
It’s unclear what Second Sight’s proposed merger means for Argus patients. The day after the merger was announced, Adam Mendelsohn, CEO of Nano Precision Medical, told Spectrum that he doesn’t yet know what contractual obligations the combined company will have to Argus and Orion patients. But, he says, NPM will try to do what’s “right from an ethical perspective.” The past, he added in an email, is “simply not relevant to the new future.”
…
There may be some alternatives, from the February 15, 2022 IEEE Spectrum article (Note: Links have been removed),
Second Sight may have given up on its retinal implant, but other companies still see a need—and a market—for bionic vision without brain surgery. Paris-based Pixium Vision is conducting European and U.S. feasibility trials to see if its Prima system can help patients with age-related macular degeneration, a much more common condition than retinitis pigmentosa.
Daniel Palanker, a professor of ophthalmology at Stanford University who licensed his technology to Pixium, says the Prima implant is smaller, simpler, and cheaper than the Argus II. But he argues that Prima’s superior image resolution has the potential to make Pixium Vision a success. “If you provide excellent vision, there will be lots of patients,” he tells Spectrum. “If you provide crappy vision, there will be very few.”
Some clinicians involved in the Argus II work are trying to salvage what they can from the technology. Gislin Dagnelie, an associate professor of ophthalmology at Johns Hopkins University School of Medicine, has set up a network of clinicians who are still working with Argus II patients. The researchers are experimenting with a thermal camera to help users see faces, a stereo camera to filter out the background, and AI-powered object recognition. These upgrades are unlikely to result in commercial hardware today but could help future vision prostheses.
…
The writers have carefully balanced this piece so it is not an outright condemnation of the companies (Second Sight and Nano Precision), from the February 15, 2022 IEEE Spectrum article,
Failure is an inevitable part of innovation. The Argus II was an innovative technology, and progress made by Second Sight may pave the way for other companies that are developing bionic vision systems. But for people considering such an implant in the future, the cautionary tale of Argus patients left in the lurch may make a tough decision even tougher. Should they take a chance on a novel technology? If they do get an implant and find that it helps them navigate the world, should they allow themselves to depend upon it?
Abandoning the Argus II technology—and the people who use it—might have made short-term financial sense for Second Sight, but it’s a decision that could come back to bite the merged company if it does decide to commercialize a brain implant, believes Doerr.
…
For anyone curious about retinal implant technology (specifically the Argus II), I have a description in a June 30, 2015 posting.
Speculations and hopes for neuroprosthetics
The field of neuroprosthetics is very active. Dr Arthur Saniotis and Prof Maciej Henneberg have written an article where they speculate about the possibilities of a neuroprosthetic that may one day merge with neurons in a February 21, 2022 Nanowerk Spotlight article,
For over a generation several types of medical neuroprosthetics have been developed, which have improved the lives of thousands of individuals. For instance, cochlear implants have restored functional hearing in individuals with severe hearing impairment.
Further advances in motor neuroprosthetics are attempting to restore motor functions in tetraplegic, limb loss and brain stem stroke paralysis subjects.
Currently, scientists are working on various kinds of brain/machine interfaces [BMI] in order to restore movement and partial sensory function. One such device is the ‘Ipsihand’ that enables movement of a paralyzed hand. The device works by detecting the recipient’s intention in the form of electrical signals, thereby triggering hand movement.
Another recent development is the 12 month BMI gait neurohabilitation program that uses a visual-tactile feedback system in combination with a physical exoskeleton and EEG operated AI actuators while walking. This program has been tried on eight patients with reported improvements in lower limb movement and somatic sensation.
Surgically placed electrode implants have also reduced tremor symptoms in individuals with Parkinson’s disease.
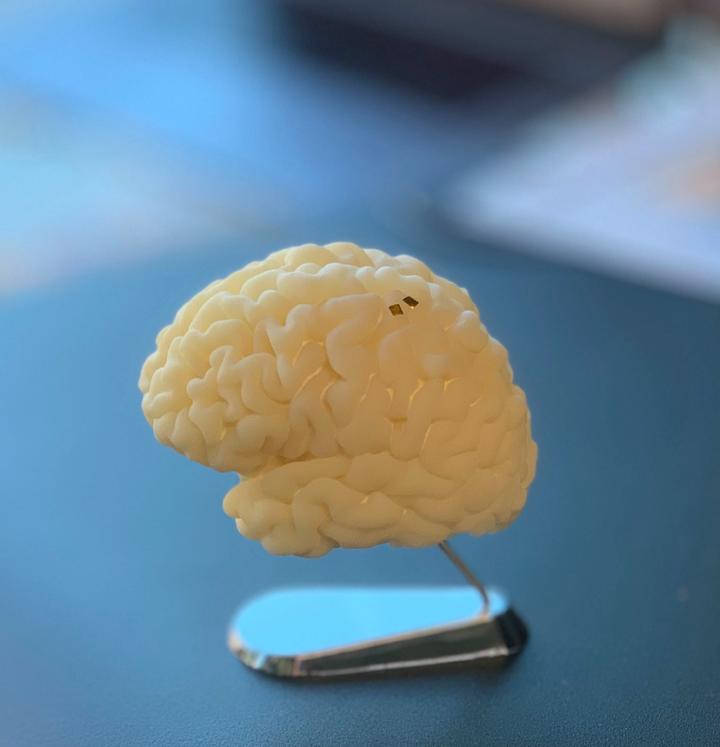
Although neuroprosthetics have provided various benefits they do have their problems. Firstly, electrode implants to the brain are prone to degradation, necessitating new implants after a few years. Secondly, as in any kind of surgery, implanted electrodes can cause post-operative infection and glial scarring. Furthermore, one study showed that the neurobiological efficacy of an implant is dependent on the rate of speed of its insertion.
But what if humans designed a neuroprosthetic, which could bypass the medical glitches of invasive neuroprosthetics? However, instead of connecting devices to neural networks, this neuroprosthetic would directly merge with neurons – a novel step. Such a neuroprosthetic could radically optimize treatments for neurodegenerative disorders and brain injuries, and possibly cognitive enhancement [emphasis mine].
A team of three international scientists has recently designed a nanobased neuroprosthetic, which was published in Frontiers in Neuroscience (“Integration of Nanobots Into Neural Circuits As a Future Therapy for Treating Neurodegenerative Disorders“). [open access paper published in 2018]
An interesting feature of their nanobot neuroprosthetic is that it has been inspired from nature by way of endomyccorhizae – a type of plant/fungus symbiosis, which is over four hundred million years old. During endomyccorhizae, fungi use numerous threadlike projections called mycelium that penetrate plant roots, forming colossal underground networks with nearby root systems. During this process fungi take up vital nutrients while protecting plant roots from infections – a win-win relationship. Consequently, the nano-neuroprosthetic has been named ‘endomyccorhizae ligand interface’, or ‘ELI’ for short.
…
The Spotlight article goes on to describe how these nanobots might function. As for the possibility of cognitive enhancement, I wonder if that might come to be described as a form of ‘artificial intelligence’.
(Dr Arthur Saniotis and Prof Maciej Henneberg are both from the Department of Anthropology, Ludwik Hirszfeld Institute of Immunology and Experimental Therapy, Polish Academy of Sciences; and Biological Anthropology and Comparative Anatomy Research Unit, Adelaide Medical School, University of Adelaide. Abdul-Rahman Sawalma who’s listed as an author on the 2018 paper is from the Palestinian Neuroscience Initiative, Al-Quds University, Beit Hanina, Palestine.)
Saniotis and Henneberg’s Spotlight article presents an optimistic view of neuroprosthetics. It seems telling that they cite cochlear implants as a success story when it is viewed by many as ethically fraught (see the Cochlear implant Wikipedia entry; scroll down to ‘Criticism and controversy’).
Ethics and your implants
This is from an April 6, 2015 article by Luc Henry on technologist.eu,
Technologist: What are the potential consequences of accepting the “augmented human” in society?
Gregor Wolbring: There are many that we might not even envision now. But let me focus on failure and obsolescence [emphasis mine], two issues that are rarely discussed. What happens when the mechanisms fails in the middle of an action? Failure has hazardous consequences, but obsolescence has psychological ones. …. The constant surgical intervention needed to update the hardware may not be feasible. A person might feel obsolete if she cohabits with others using a newer version.
T. Are researchers working on prosthetics sometimes disconnected from reality?
G. W. Students engaged in the development of prosthetics have to learn how to think in societal terms and develop a broader perspective. Our education system provides them with a fascination for clever solutions to technological challenges but not with tools aiming at understanding the consequences, such as whether their product might increase or decrease social justice.
…
Wolbring is a professor at the University of Calgary’s Cumming School of Medicine (profile page) who writes on social issues to do with human enhancement/ augmentation. As well,
Some of his areas of engagement are: ability studies including governance of ability expectations, disability studies, governance of emerging and existing sciences and technologies (e.g. nanoscale science and technology, molecular manufacturing, aging, longevity and immortality, cognitive sciences, neuromorphic engineering, genetics, synthetic biology, robotics, artificial intelligence, automatization, brain machine interfaces, sensors), impact of science and technology on marginalized populations, especially people with disabilities he governance of bodily enhancement, sustainability issues, EcoHealth, resilience, ethics issues, health policy issues, human rights and sport.
He also maintains his own website here.
Not just startups
I’d classify Second Sight as a tech startup company and they have a high rate of failure, which may not have been clear to the patients who had the implants. Clinical trials can present problems too as this excerpt from my September 17, 2020 posting notes,
This October 31, 2017 article by Emily Underwood for Science was revelatory,
“In 2003, neurologist Helen Mayberg of Emory University in Atlanta began to test a bold, experimental treatment for people with severe depression, which involved implanting metal electrodes deep in the brain in a region called area 25 [emphases mine]. The initial data were promising; eventually, they convinced a device company, St. Jude Medical in Saint Paul, to sponsor a 200-person clinical trial dubbed BROADEN.
This month [October 2017], however, Lancet Psychiatry reported the first published data on the trial’s failure. The study stopped recruiting participants in 2012, after a 6-month study in 90 people failed to show statistically significant improvements between those receiving active stimulation and a control group, in which the device was implanted but switched off.
…
… a tricky dilemma for companies and research teams involved in deep brain stimulation (DBS) research: If trial participants want to keep their implants [emphases mine], who will take responsibility—and pay—for their ongoing care? And participants in last week’s meeting said it underscores the need for the growing corps of DBS researchers to think long-term about their planned studies.”
Symbiosis can be another consequence, as mentioned in my September 17, 2020 posting,
From a July 24, 2019 article by Liam Drew for Nature Outlook: The brain,
“It becomes part of you,” Patient 6 said, describing the technology that enabled her, after 45 years of severe epilepsy, to halt her disabling seizures. Electrodes had been implanted on the surface of her brain that would send a signal to a hand-held device when they detected signs of impending epileptic activity. On hearing a warning from the device, Patient 6 knew to take a dose of medication to halt the coming seizure.
“You grow gradually into it and get used to it, so it then becomes a part of every day,” she told Frederic Gilbert, an ethicist who studies brain–computer interfaces (BCIs) at the University of Tasmania in Hobart, Australia. “It became me,” she said. [emphasis mine]
…
Symbiosis is a term, borrowed from ecology, that means an intimate co-existence of two species for mutual advantage. As technologists work towards directly connecting the human brain to computers, it is increasingly being used to describe humans’ potential relationship with artificial intelligence. [emphasis mine]
…
It’s complicated
For a lot of people these devices are or could be life-changing. At the same time, there are a number of different issues related to implants/prosthetics; the following is not an exhaustive list. As Wolbring notes, issues that we can’t begin to imagine now are likely to emerge as these medical advances become more ubiquitous.
Ability/disability?
Assistive technologies are almost always portrayed as helpful. For example, a cochlear implant gives people without hearing the ability to hear. The assumption is that this is always a good thing—unless you’re a deaf person who wants to define the problem a little differently. Who gets to decide what is good and ‘normal’ and what is desirable?
While the cochlear implant is the most extreme example I can think of, there are variations of these questions throughout the ‘disability’ communities.
Also, as Wolbring notes in his interview with the Technologist.eu, the education system tends to favour technological solutions which don’t take social issues into account. Wolbring cites social justice issues when he mentions failure and obsolescence.
Technical failures and obsolescence
The story, excerpted earlier in this posting, opened with a striking example of a technical failure at an awkward moment; a blind woman depending on her retinal implant loses all sight as she maneuvers through a subway station in New York City.
Aside from being an awful way to find out the company supplying and supporting your implant is in serious financial trouble and can’t offer assistance or repair, the failure offers a preview of what could happen as implants and prosthetics become more commonly used.
Keeping up/fomo (fear of missing out)/obsolescence
It used to be called ‘keeping up with the Joneses, it’s the practice of comparing yourself and your worldly goods to someone else(‘s) and then trying to equal what they have or do better. Usually, people want to have more and better than the mythical Joneses.
These days, the phenomenon (which has been expanded to include social networking) is better known as ‘fomo’ or fear of missing out (see the Fear of missing out Wikipedia entry).
Whatever you want to call it, humanity’s competitive nature can be seen where technology is concerned. When I worked in technology companies, I noticed that hardware and software were sometimes purchased for features that were effectively useless to us. But, not upgrading to a newer version was unthinkable.
Call it fomo or ‘keeping up with the Joneses’, it’s a powerful force and when people (and even companies) miss out or can’t keep up, it can lead to a sense of inferiority in the same way that having an obsolete implant or prosthetic could.
Social consequences
Could there be a neural implant/neuroprosthetic divide? There is already a digital divide (from its Wikipedia entry),
The digital divide is a gap between those who have access to new technology and those who do not … people without access to the Internet and other ICTs [information and communication technologies] are at a socio-economic disadvantage because they are unable or less able to find and apply for jobs, shop and sell online, participate democratically, or research and learn.
…
After reading Wolbring’s comments, it’s not hard to imagine a neural implant/neuroprosthetic divide with its attendant psychological and social consequences.
What kind of human am I?
There are other issues as noted in my September 17, 2020 posting. I’ve already mentioned ‘patient 6’, the woman who developed a symbiotic relationship with her brain/computer interface. This is how the relationship ended,
… He [Frederic Gilbert, ethicist] is now preparing a follow-up report on Patient 6. The company that implanted the device in her brain to help free her from seizures went bankrupt. The device had to be removed.
… Patient 6 cried as she told Gilbert about losing the device. … “I lost myself,” she said.
“It was more than a device,” Gilbert says. “The company owned the existence of this new person.”
…
Above human
The possibility that implants will not merely restore or endow someone with ‘standard’ sight or hearing or motion or … but will augment or improve on nature was broached in this May 2, 2013 posting, More than human—a bionic ear that extends hearing beyond the usual frequencies and is one of many in the ‘Human Enhancement’ category on this blog.
More recently, Hugh Herr, an Associate Professor at the Massachusetts Institute of Technology (MIT), leader of the Biomechatronics research group at MIT’s Media Lab, a double amputee, and prosthetic enthusiast, starred in the recent (February 23, 2022) broadcast of ‘Augmented‘ on the Public Broadcasting Service (PBS) science programme, Nova.
I found ‘Augmented’ a little offputting as it gave every indication of being an advertisement for Herr’s work in the form of a hero’s journey. I was not able to watch more than 10 mins. This preview gives you a pretty good idea of what it was like although the part in ‘Augmented, where he says he’d like to be a cyborg hasn’t been included,
At a guess, there were a few talking heads (taking up from 10%-20% of the running time) who provided some cautionary words to counterbalance the enthusiasm in the rest of the programme. It’s a standard approach designed to give the impression that both sides of a question are being recognized. The cautionary material is usually inserted past the 1/2 way mark while leaving several minutes at the end for returning to the more optimistic material.
In a February 2, 2010 posting I have excerpts from an article featuring quotes from Herr that I still find startling,
Written by Paul Hochman for Fast Company, Bionic Legs, iLimbs, and Other Super-Human Prostheses [ETA March 23, 2022: an updated version of the article is now on Genius.com] delves further into the world where people may be willing to trade a healthy limb for a prosthetic. From the article,
There are many advantages to having your leg amputated.
Pedicure costs drop 50% overnight. A pair of socks lasts twice as long. But Hugh Herr, the director of the Biomechatronics Group at the MIT Media Lab, goes a step further. “It’s actually unfair,” Herr says about amputees’ advantages over the able-bodied. “As tech advancements in prosthetics come along, amputees can exploit those improvements. They can get upgrades. A person with a natural body can’t.”
…
Herr is not the only one who favours prosthetics (also from the Hochman article),
This influx of R&D cash, combined with breakthroughs in materials science and processor speed, has had a striking visual and social result: an emblem of hurt and loss has become a paradigm of the sleek, modern, and powerful. Which is why Michael Bailey, a 24-year-old student in Duluth, Georgia, is looking forward to the day when he can amputate the last two fingers on his left hand.
“I don’t think I would have said this if it had never happened,” says Bailey, referring to the accident that tore off his pinkie, ring, and middle fingers. “But I told Touch Bionics I’d cut the rest of my hand off if I could make all five of my fingers robotic.”
…
But Bailey is most surprised by his own reaction. “When I’m wearing it, I do feel different: I feel stronger. As weird as that sounds, having a piece of machinery incorporated into your body, as a part of you, well, it makes you feel above human.[emphasis mine] It’s a very powerful thing.”
…
My September 17, 2020 posting touches on more ethical and social issues including some of those surrounding consumer neurotechnologies or brain-computer interfaces (BCI). Unfortunately, I don’t have space for these issues here.
As for Paul Hochman’s article, Bionic Legs, iLimbs, and Other Super-Human Prostheses, now on Genius.com, it has been updated.
Money makes the world go around
Money and business practices have been indirectly referenced (for the most part) up to now in this posting. The February 15, 2022 IEEE Spectrum article and Hochman’s article, Bionic Legs, iLimbs, and Other Super-Human Prostheses, cover two aspects of the money angle.
In the IEEE Spectrum article, a tech start-up company, Second Sight, ran into financial trouble and is acquired by a company that has no plans to develop Second Sight’s core technology. The people implanted with the Argus II technology have been stranded as were ‘patient 6’ and others participating in the clinical trial described in the July 24, 2019 article by Liam Drew for Nature Outlook: The brain mentioned earlier in this posting.
I don’t know anything about the business bankruptcy mentioned in the Drew article but one of the business problems described in the IEEE Spectrum article suggests that Second Sight was founded before answering a basic question, “What is the market size for this product?”
On 18 July 2019, Second Sight sent Argus patients a letter saying it would be phasing out the retinal implant technology to clear the way for the development of its next-generation brain implant for blindness, Orion, which had begun a clinical trial with six patients the previous year. …
“The leadership at the time didn’t believe they could make [the Argus retinal implant] part of the business profitable,” Greenberg [Robert Greenberg, Second Sight co-founder] says. “I understood the decision, because I think the size of the market turned out to be smaller than we had thought.”
….
The question of whether a medical procedure or medicine can be profitable (or should the question be sufficiently profitable?) was referenced in my April 26, 2019 posting in the context of gene editing and personalized medicine
Edward Abrahams, president of the Personalized Medicine Coalition (US-based), advocates for personalized medicine while noting in passing, market forces as represented by Goldman Sachs in his May 23, 2018 piece for statnews.com (Note: A link has been removed),
…
Goldman Sachs, for example, issued a report titled “The Genome Revolution.” It argues that while “genome medicine” offers “tremendous value for patients and society,” curing patients may not be “a sustainable business model.” [emphasis mine] The analysis underlines that the health system is not set up to reap the benefits of new scientific discoveries and technologies. Just as we are on the precipice of an era in which gene therapies, gene-editing, and immunotherapies promise to address the root causes of disease, Goldman Sachs says that these therapies have a “very different outlook with regard to recurring revenue versus chronic therapies.”
…
The ‘Glybera’ story in my July 4, 2019 posting (scroll down about 40% of the way) highlights the issue with “recurring revenue versus chronic therapies,”
Kelly Crowe in a November 17, 2018 article for the CBC (Canadian Broadcasting Corporation) news writes about Glybera,
It is one of this country’s great scientific achievements.
“The first drug ever approved that can fix a faulty gene.
It’s called Glybera, and it can treat a painful and potentially deadly genetic disorder with a single dose — a genuine made-in-Canada medical breakthrough.
But most Canadians have never heard of it.…
Here’s my summary (from the July 4, 2019 posting),
…
It cost $1M for a single treatment and that single treatment is good for at least 10 years.
Pharmaceutical companies make their money from repeated use of their medicaments and Glybera required only one treatment so the company priced it according to how much they would have gotten for repeated use, $100,000 per year over a 10 year period. The company was not able to persuade governments and/or individuals to pay the cost
In the end, 31 people got the treatment, most of them received it for free through clinical trials.
…
For rich people only?
Megan Devlin’s March 8, 2022 article for the Daily Hive announces a major research investment into medical research (Note: A link has been removed),
Vancouver [Canada] billionaire Chip Wilson revealed Tuesday [March 8, 2022] that he has a rare genetic condition that causes his muscles to waste away, and announced he’s spending $100 million on research to find a cure.
His condition is called facio-scapulo-humeral muscular dystrophy, or FSHD for short. It progresses rapidly in some people and more slowly in others, but is characterized by progressive muscle weakness starting the the face, the neck, shoulders, and later the lower body.
“I’m out for survival of my own life,” Wilson said.
“I also have the resources to do something about this which affects so many people in the world.”
…
Wilson hopes the $100 million will produce a cure or muscle-regenerating treatment by 2027.
“This could be one of the biggest discoveries of all time, for humankind,” Wilson said. “Most people lose muscle, they fall, and they die. If we can keep muscle as we age this can be a longevity drug like we’ve never seen before.”
…
According to rarediseases.org, FSHD affects between four and 10 people out of every 100,000 [emphasis mine], Right now, therapies are limited to exercise and pain management. There is no way to stall or reverse the disease’s course.
…
Wilson is best known for founding athleisure clothing company Lululemon. He also owns the most expensive home in British Columbia, a $73 million mansion in Vancouver’s Kitsilano neighbourhood.
Let’s see what the numbers add up to,
4 – 10 people out of 100,000
40 – 100 people out of 1M
1200 – 3,000 people out of 30M (let’s say this is Canada’s population)\
12,000 – 30,000 people out of 300M (let’s say this is the US’s population)
42,000 – 105,000 out of 1.115B (let’s say this is China’s population)
The rough total comes to 55,200 to 138,000 people between three countries with a combined population total of 1.445B. Given how business currently operates, it seems unlikely that any company will want to offer Wilson’s hoped for medical therapy although he and possibly others may benefit from a clinical trial.
Should profit or wealth be considerations?
The stories about the patients with the implants and the patients who need Glybera are heartbreaking and point to a question not often asked when medical therapies and medications are developed. Is the profit model the best choice and, if so, how much profit?
I have no answer to that question but I wish it was asked by medical researchers and policy makers.
As for wealthy people dictating the direction for medical research, I don’t have answers there either. I hope the research will yield applications and/or valuable information for more than Wilson’s disease.
It’s his money after all
Wilson calls his new venture, SolveFSHD. It doesn’t seem to be affiliated with any university or biomedical science organization and it’s not clear how the money will be awarded (no programmes, no application procedure, no panel of experts). There are three people on the team, Eva R. Chin, scientist and executive director, Chip Wilson, SolveFSHD founder/funder, and FSHD patient, and Neil Camarta, engineer, executive (fossil fuels and clean energy), and FSHD patient. There’s also a Twitter feed (presumably for the latest updates): https://twitter.com/SOLVEFSHD.
Perhaps unrelated but intriguing is news about a proposed new building in Kenneth Chan’s March 31, 2022 article for the Daily Hive,
Low Tide Properties, the real estate arm of Lululemon founder Chip Wilson [emphasis mine], has submitted a new development permit application to build a 148-ft-tall, eight-storey, mixed-use commercial building in the False Creek Flats of Vancouver.
…
The proposal, designed by local architectural firm Musson Cattell Mackey Partnership, calls for 236,000 sq ft of total floor area, including 105,000 sq ft of general office space, 102,000 sq ft of laboratory space [emphasis mine], and 5,000 sq ft of ground-level retail space. An outdoor amenity space for building workers will be provided on the rooftop.
…
[next door] The 2001-built, five-storey building at 1618 Station Street immediately to the west of the development site is also owned by Low Tide Properties [emphasis mine]. The Ferguson, the name of the existing building, contains about 79,000 sq ft of total floor area, including 47,000 sq ft of laboratory space and 32,000 sq ft of general office space. Biotechnology company Stemcell technologies [STEMCELL] Technologies] is the anchor tenant [emphasis mine].
…
I wonder if this proposed new building will house SolveFSHD and perhaps other FSHD-focused enterprises. The proximity of STEMCELL Technologies could be quite convenient. In any event, $100M will buy a lot (pun intended).
The end
Issues I’ve described here in the context of neural implants/neuroprosthetics and cutting edge medical advances are standard problems not specific to these technologies/treatments:
- What happens when the technology fails (hopefully not at a critical moment)?
- What happens when your supplier goes out of business or discontinues the products you purchase from them?
- How much does it cost?
- Who can afford the treatment/product? Will it only be for rich people?
- Will this technology/procedure/etc. exacerbate or create new social tensions between social classes, cultural groups, religious groups, races, etc.?
Of course, having your neural implant fail suddenly in the middle of a New York City subway station seems a substantively different experience than having your car break down on the road.
There are, of course, there are the issues we can’t yet envision (as Wolbring notes) and there are issues such as symbiotic relationships with our implants and/or feeling that you are “above human.” Whether symbiosis and ‘implant/prosthetic superiority’ will affect more than a small number of people or become major issues is still to be determined.
There’s a lot to be optimistic about where new medical research and advances are concerned but I would like to see more thoughtful coverage in the media (e.g., news programmes and documentaries like ‘Augmented’) and more thoughtful comments from medical researchers.
Of course, the biggest issue I’ve raised here is about the current business models for health care products where profit is valued over people’s health and well-being. it’s a big question and I don’t see any definitive answers but the question put me in mind of this quote (from a September 22, 2020 obituary for US Supreme Court Justice Ruth Bader Ginsburg by Irene Monroe for Curve),
Ginsburg’s advocacy for justice was unwavering and showed it, especially with each oral dissent. In another oral dissent, Ginsburg quoted a familiar Martin Luther King Jr. line, adding her coda:” ‘The arc of the universe is long, but it bends toward justice,’” but only “if there is a steadfast commitment to see the task through to completion.” …
Martin Luther King Jr. popularized and paraphrased the quote (from a January 18, 2018 article by Mychal Denzel Smith for Huffington Post),
…
His use of the quote is best understood by considering his source material. “The arc of the moral universe is long, but it bends toward justice” is King’s clever paraphrasing of a portion of a sermon delivered in 1853 by the abolitionist minister Theodore Parker. Born in Lexington, Massachusetts, in 1810, Parker studied at Harvard Divinity School and eventually became an influential transcendentalist and minister in the Unitarian church. In that sermon, Parker said: “I do not pretend to understand the moral universe. The arc is a long one. My eye reaches but little ways. I cannot calculate the curve and complete the figure by experience of sight. I can divine it by conscience. And from what I see I am sure it bends toward justice.”
…
I choose to keep faith that people will get the healthcare products they need and that all of us need to keep working at making access more fair.