A June 25, 2014 news item on Nanowerk highlights PneumoNP a new European Union ‘theragnostic’ research project (Note: Links have been removed) ,
A new research project (PneumoNP) is aimed at tackling antibiotic resistance in respiratory tract infections via the use of inhalable nanotherapeutic compounds. Funded under the FP7 programme by the European Commission, the 4-year long PneumoNP project brings together top research institutes, universities, clinicians and enterprises from 6 EU member states. This novel collaboration will contribute to answer the call of the World Health Organization (WHO), who recently released an alarming report on the global threat of antibiotic resistance.
The project will develop an innovative solution to antibiotic resistance by coupling new antibiotics to inhalable carrier molecules, resulting in more efficient targeting of antibiotics to infection-causing bacteria present in the respiratory tract.
An April 30, 2014 WHO news release details the level of antibiotic resistance,
New WHO report provides the most comprehensive picture of antibiotic resistance to date, with data from 114 countries
A new report by WHO–its first to look at antimicrobial resistance, including antibiotic resistance, globally–reveals that this serious threat is no longer a prediction for the future, it is happening right now in every region of the world and has the potential to affect anyone, of any age, in any country. Antibiotic resistance–when bacteria change so antibiotics no longer work in people who need them to treat infections–is now a major threat to public health.
…
The report, “Antimicrobial resistance: global report on surveillance”, notes that resistance is occurring across many different infectious agents but the report focuses on antibiotic resistance in seven different bacteria responsible for common, serious diseases such as bloodstream infections (sepsis), diarrhoea, pneumonia, urinary tract infections and gonorrhoea. The results are cause for high concern, documenting resistance to antibiotics, especially “last resort” antibiotics, in all regions of the world.Key findings from the report include:
Resistance to the treatment of last resort for life-threatening infections caused by a common intestinal bacteria, Klebsiella pneumoniae–carbapenem antibiotics–has spread to all regions of the world. K. pneumoniae is a major cause of hospital-acquired infections such as pneumonia, bloodstream infections, infections in newborns and intensive-care unit patients. In some countries, because of resistance, carbapenem antibiotics would not work in more than half of people treated for K. pneumoniae infections.
Resistance to one of the most widely used antibacterial medicines for the treatment of urinary tract infections caused by E. coli–fluoroquinolones–is very widespread. In the 1980s, when these drugs were first introduced, resistance was virtually zero. Today, there are countries in many parts of the world where this treatment is now ineffective in more than half of patients.
Treatment failure to the last resort of treatment for gonorrhoea–third generation cephalosporins–has been confirmed in Austria, Australia, Canada, France, Japan, Norway, Slovenia, South Africa, Sweden and the United Kingdom. More than 1 million people are infected with gonorrhoea around the world every day.
Antibiotic resistance causes people to be sick for longer and increases the risk of death. For example, people with MRSA (methicillin-resistant Staphylococcus aureus) are estimated to be 64% more likely to die than people with a non-resistant form of the infection. Resistance also increases the cost of health care with lengthier stays in hospital and more intensive care required.
The suggestions offered for tackling antibiotic resistance will be familiar to many (from the news release),
People can help tackle resistance by:
- using antibiotics only when prescribed by a doctor;
- completing the full prescription, even if they feel better;
- never sharing antibiotics with others or using leftover prescriptions.
A June 25, 2014 PneumoNP press release describes both the European Union’s response to massive, global antibiotic resistance and the specifics of the new programme (PneumoNP),
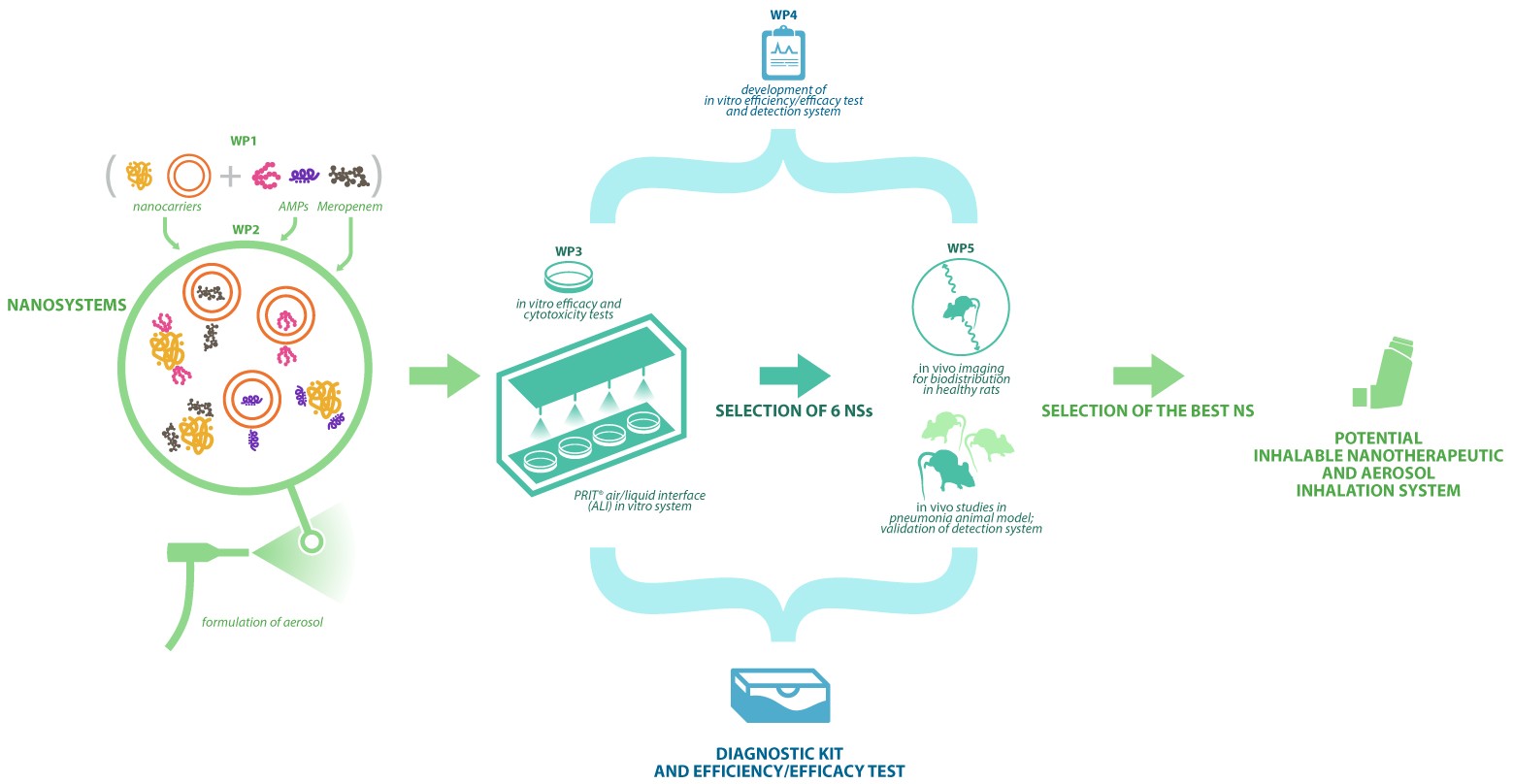
In this context, the European Commission launched 15 projects under its7 Framework Programme to fight antimicrobial resistance, with PneumoNP being one of these projects. Started in 2014, the aim of this 4-year project is to develop novel therapeutic and diagnostic tools for bacterial respiratory tract infections, focusing on infections caused by Klebsiella pneumoniae. PneumoNP will pioneer the development of a therapeutic treatment based on a combination of nanocarriers coupled to new antibiotics. This novel combination is expected to enhance the efficiency of antibiotic delivery to the patient. The project is expected to generate:
- a new inhalable drug system made of a new nanotherapeutic system (an antimicrobial peptide or an active pharmaceutical ingredient and a nanocarrier);
- a new aerosol technology that will allow direct access to the main focus of infection;
- an innovative efficiency-efficacy test to follow-up the treatment;
- a new diagnostic test for faster detection and identification of antibiotic resistance in bacteria causing respiratory infections.
…
European funding allows PneumoNP to combine scientific research capacities with the expert healthcare capabilities of European enterprises. The result is an interdisciplinary collaboration between 11 teams from 6 EU member states – Spain, Italy, France, Germany, The Netherlands, and Denmark. Each partner has a distinct yet collaborative role according to its own expertise involving a total of 8 work packages.
There is a figure in the news release which illustrates the PneumoNP concept,
There is more information about PneumoNP on its website. I wasn’t able to glean much in the way of technical details (are they using silver nanoparticles, what kind of nanocarriers are they considering, etc.) but I imagine those will emerge with time. There is this from the homepage which features the relatively new (to me) word, theragnostic,
Development of a theragnostic system for the treatment of lung Gram-negative bacterial infections
I assume they are conflating two processes, therapeutics and diagnostics for theragnostics.