The latest research does not lead to a magical disease detector where nanoscale sensors swim through the body continuously monitoring our health and alerting us should something untoward occur (see this Oct. 28, 2014 article on RT.com for more about Google X’s development plans for it and this Nov. 11, 2015 news item on Nanowerk for a measured response from a researcher in the field).
Now onto some real research, a Nov. 17, 2015 news item on ScienceDaily announces an ultrasensitive (attoscale) sensor employing gold nanoparticles for detecting cancer,
A simple, ultrasensitive microRNA sensor developed and tested by researchers from the schools of science and medicine at Indiana University-Purdue University Indianapolis and the Indiana University Melvin and Bren Simon Cancer Center holds promise for the design of new diagnostic strategies and, potentially, for the prognosis and treatment of pancreatic and other cancers.
A Nov. 17, 2015 Indiana University-Purdue University Indianapolis news release on EurekAlert, which originated the news item, provides more detail about research that seems to have focused largely on pancreatic cancer detection (Note: Links have been removed),
In a study published in the Nov. [2015] issue of ACS Nano, a peer-reviewed journal of the American Chemical Society focusing on nanoscience and nanotechnology research, the IUPUI researchers describe their design of the novel, low-cost, nanotechnology-enabled reusable sensor. They also report on the promising results of tests of the sensor’s ability to identify pancreatic cancer or indicate the existence of a benign condition by quantifying changes in levels of microRNA signatures linked to pancreatic cancer. MicroRNAs are small molecules of RNA that regulate how larger RNA molecules lead to protein expression. As such, microRNAs are very important in biology and disease states.
“We used the fundamental concepts of nanotechnology to design the sensor to detect and quantify biomolecules at very low concentrations,” said Rajesh Sardar, Ph.D., who developed the sensor.
“We have designed an ultrasensitive technique so that we can see minute changes in microRNA concentrations in a patient’s blood and confirm the presence of pancreatic cancer.” Sardar is an assistant professor of chemistry and chemical biology in the School of Science at IUPUI and leads an interdisciplinary research program focusing on the intersection of analytical chemistry and the nanoscience of metallic nanoparticles.
“If we can establish that there is cancer in the pancreas because the sensor detects high levels of microRNA-10b or one of the other microRNAs associated with that specific cancer, we may be able to treat it sooner,” said Murray Korc, M.D., the Myles Brand Professor of Cancer Research at the IU School of Medicine and a researcher at the IU Simon Cancer Center. Korc, worked with Sardar to improve the sensor’s capabilities and led the testing of the sensor and its clinical uses as well as advancing the understanding of pancreatic cancer biology.
“That’s especially significant for pancreatic cancer, because for many patients it is symptom-free for years or even a decade or more, by which time it has spread to other organs, when surgical removal is no longer possible and therapeutic options are limited,” said Korc. “For example, diagnosis of pancreatic cancer at an early stage of the disease followed by surgical removal is associated with a 40 percent five-year survival. Diagnosis of metastatic pancreatic cancer, by contrast, is associated with life expectancy that is often only a year or less.
“The beauty of the sensor designed by Dr. Sardar is its ability to accurately detect mild increases in microRNA levels, which could allow for early cancer diagnosis,” Korc added.
Over the past decade, studies have shown that microRNAs play important roles in cancer and other diseases, such as diabetes and cardiovascular disorders. The new IUPUI nanotechnology-based sensor can detect changes in any of these microRNAs.
The sensor is a small glass chip that contains triangular-shaped gold nanoparticles called ‘nanoprisms.’ After dipping it in a sample of blood or another body fluid, the scientist measures the change in the nanoprism’s optical property to determine the levels of specific microRNAs.
For anyone concerned about the cost associated with creating sensors based on gold, about patents, or about current techniques for monitoring microRNAs, there’s more from the news release (Note: A link has been removed),
“Using gold nanoprisms may sound expensive, but it isn’t because these particles are so very tiny,” Sardar said. “It’s a rather cheap technique because it uses nanotechnology and needs very little gold. $250 worth of gold makes 4,000 sensors. Four thousand sensors allow you to do at least 4,000 tests. The low cost makes this technique ideal for use anywhere, including in low-resource environments in this country and around the world.”
Indiana University Research and Technology Corporation has filed a patent application on Sardar’s and Korc’s groundbreaking nanotechnology-enabled sensor. The researchers’ ultimate goal is to design ultrasensitive and extremely selective low-cost point-of-care diagnostics enabling individual therapeutic approaches to diseases.
Currently, polymerase chain reaction technology is used to determine microRNA signatures, which requires extraction of the microRNA from blood or other biological fluid and reverse transcription or amplification of the microRNA. PCR provides relative values. By contrast, the process developed at IUPUI is simpler, quantitative, more sensitive and highly specific even when two different microRNAs vary in a single position. The study demonstrated that the IUPUI nanotechnology-enabled sensor is as good as if not better than the most advanced PCR in detection and quantification of microRNA.
Here’s a link to and a citation for the paper,
Label-Free Nanoplasmonic-Based Short Noncoding RNA Sensing at Attomolar Concentrations Allows for Quantitative and Highly Specific Assay of MicroRNA-10b in Biological Fluids and Circulating Exosomes by Gayatri K. Joshi, Samantha Deitz-McElyea, Thakshila Liyanage, Katie Lawrence, Sonali Mali, Rajesh Sardar*, and Murray Korc. ACS Nano, Article ASAP DOI: 10.1021/acsnano.5b04527 Publication Date (Web): October 7, 2015
Copyright © 2015 American Chemical Society
This is an open access paper.
The researchers have provided this illustration of gold nanoprisms,
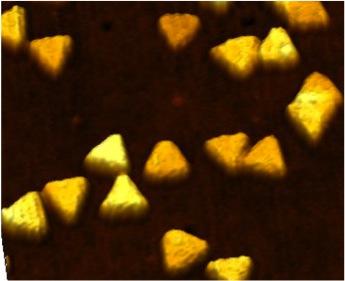
Caption: Indiana University-Purdue University Indianapolis researchers have developed a novel, low-cost, nanotechnology-enabled reusable sensor for which a patent application has been filed. Credit: Department of Chemistry and Chemical Biology, School of Science, Indiana University-Purdue University Indianapolis