I got curious the other day about trachea transplants, a topic I first wrote about one an Aug. 22, 2011 posting featuring Andemariam Teklesenbet Beyene and wondered how things had worked out for him. For anyone who doesn’t know the story, ,
In early July 2011, there were reports of a new kind of transplant involving a body part made of a biocomposite. Andemariam Teklesenbet Beyene underwent a trachea transplant that required an artificial windpipe crafted by UK experts then flown to Sweden where Beyene’s stem cells were used to coat the windpipe before being transplanted into his body.
It is an extraordinary story not least because Beyene, a patient in a Swedish hospital planning to return to Eritrea after his PhD studies in Iceland, illustrates the international cooperation that made the transplant possible.
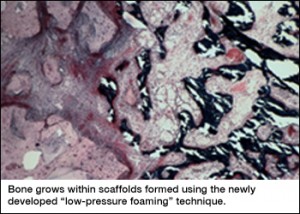
The scaffolding material for the artificial windpipe was developed by Professor Alex Seifalian at the University College London in a landmark piece of nanotechnology-enabled tissue engineering. Tim Harper in his July 25, 2011 posting provides more details about the scaffolding,
A team led by Professor Alexander Seifalian (UCL Division of Surgery & Interventional Science; professor of nanotechnology and regenerative medicine at University College London, UK), whose laboratories are headquartered at the Royal Free Hospital, created a glass mold of the patient’s trachea from X-ray computed tomography (CT) scans of the patient. In CT, digital geometry processing is employed to generate a 3D image of the inside of an object from a large series of 2D X-ray images taken around one single axis of rotation.
Then, they manufactured a full size y-shaped trachea scaffold at Professor Seifalian’s laboratories. The scaffold of the trachea was built using a novel nanocomposite polymer developed and patented by Professor Seifalian. Professor Seifalian worked together with Professor Paolo Macchiarini at Karolinska Institutet, Stockholm, Sweden (who also holds an Honorary appointment at UCL).
…
What I didn’t realize in 2011 was there had been some earlier transplants as Gretchen Vogel writes in her April 19, 2013 article (Trachea Transplants Test the Limits) which summarizes and critiques the work* on synthesized tracheas to date for Science magazine (the article is behind a a paywall),
More than a dozen ill people have received a bioengineered trachea seeded with stem cells during the past 5 years, but outcomes are mixed, and critics say the treatment may not do what its developers claim.
…
Although at first glance the trachea might seem like a simple tube, its thin but cartilage-reinforced walls must stand up to near-constant use as a person breathes, clears his throat, or coughs. Any transplant, therefore, has to be strong enough to withstand such pressures without collapsing. But a rigid prosthesis can rub against and damage the adjacent major blood vessels in the upper part of the chest, leaving a patient at risk for a fatal hemorrhage. At the same time, the natural blood supply for the trachea’s tissues is intricate, with vessels too small for surgeons to easily reconnect during a transplant operation. And because it is exposed to inhaled air, the wound between the implant and the remaining airway is especially vulnerable to infection.
Surgeons have tried for years to find ways around these challenges, without much success. When Castillo (Claudia Castillo, first patient to receive a trachea transplant using her own stem cells) was hospitalized in Barcelona in March 2008, Macchiarini [Paolo Macchiarini], who was then at the University of Barcelona’s Hospital Clínic, and Birchall [Martin Birchall], then at the University of Bristol in the United Kingdom, had experimented with bioengineered transplants in pigs. They would take a trachea from a pig and remove its living cells to create a so-called decellularized scaffold. They seeded this with cells from the recipient pig: bone marrow cells on the outer layer, thought to help form new cartilage, and epithelial cells on the inside, which they hoped would regrow the trachea’s lining. They allowed the cells to grow on the scaffold for several days in a bioreactor designed to provide different conditions for the two types of cells. They hoped that the decellularized scaffold would not require immunosuppressive drugs to prevent its rejection and that the seeded cells would take over the removed cells’ roles, ultimately forming a living organ.
The main difference between the 2008 Castillo operation and the 2011 Teklesenbet Beyene,operation is the scaffolding. For Castillo, they used a cadaverous** trachea where living cells were removed to create a ‘decellularized’ scaffold. For Teklesenbet Beyene, they used a nanocomposite** polymer. According to Vogel, 14 people have had the operation using either the decellularized or the nanocomposite composite polymer as the base for a new trachea. There have been some problems and deaths although Castillo who is still alive did not respond to any of Vogel’s requests for a comment . As for Teklesenbet Beyene (from the article),
His current doctor, Tomas Gudbjartsson of Landspitali University Hospital in Reykjavik, tells Science that Beyene has had several stents, but is healthy enough that he was able to complete his studies last year [2012]. The researchers have mentioned other patients in passing in several papers, but no formal reports have been published about their health, and Science has not been able to independently verify the current status of all the patients.
Both Birchall and Macchiarini have received grants for clinical trials,
In March [2013?[, Birchall received a £2.8 million ($4.3 million) grant from the United Kingdom’s Medical Research Council to conduct a trial of decellularized and stem cell–seeded upper trachea and larynx, with roughly 10 patients. Macchiarini has already completed two transplants in Russia as part of a clinical trial—funded with a $6 million grant from the Russian government—that he says should eventually enroll 20 or 25 patients. “We were allowed to do this type of transplantation only in extreme cases,” he says. “The clinical study for the first time gives us a chance to include patients who are not in such critical shape.”
Macchiarini is also the lead investigator on a 5-year, €4 million ($5.2 million) grant from the European Union to begin a clinical trial using decellularized tracheas and further develop the polymer scaffolds in large animal models. That project may need to be reorganized, however, following a legal dispute last year in Italy, where the transplants were supposed to take place—Macchiarini had a part-time position at Careggi Hospital in Florence. In September, however, Italy’s financial police accused him of attempted extortion, and briefly placed him under house arrest, for allegedly telling a patient that he could receive treatment in Germany for €150,000. Macchiarini and his lawyer say that he was simply informing the patient of possible options, not demanding payment. The main charges were soon dropped, but Macchiarini says that the charges stemmed from academic politics in Tuscany and he has severed ties with the hospital and university there. “There is no way to go back there.”
That last bit (in the excerpt) about academic politics in Tuscany seems downright Machiavellian (Wikipedia essay on Machiavelli here).
Getting back to the trachea transplants, there seems to be a major difference of opinion. While the researchers Macchiarini and Birchall have opted for human clinical trials other experts are suggesting that animal trials should be the next step for this research. I recommend reading Vogel’s article so you can fully appreciate the debate.
*’which a summary and critique of the work’ changed to ‘which summarizes and critiques the work’ for grammatical correctness on April 8, 2016.
**’pig trachea’ changed to ‘cadaverous trachea’ and ‘nanocompostie’ changed to ‘nanocomposite’ on April 19, 2016.