Since the international July 2011 coverage of Andemariam Teklesenbet Beyene’s synthetic trachea transplant (mentioned in my Aug. 2, 2011 posting), I’ve been quite interested in tissue engineering. Scientists at Northwestern University (US) have developed a new type of scaffolding for tissue engineering.
There’s a description in the Feb. 12, 2012 news release on EurekAlert of tissue engineering and scaffolding and some of the disadvantages with the current technology,
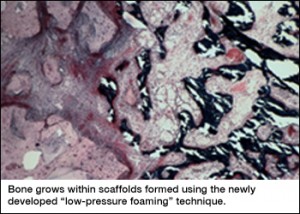
Through tissue engineering, researchers seek to regenerate human tissue, such as bone and cartilage, that has been damaged by injury or disease. Scaffolds — artificial, lattice-like structures capable of supporting tissue formation — are necessary in this process to provide a template to support the growing cells. Over time, the scaffold resorbs into the body, leaving behind the natural tissue.
Scaffolds are typically engineered with pores that allow the cells to migrate throughout the material. The pores are often created with the use of salt, sugar, or carbon dioxide gas, but these additives have various drawbacks; They create an imperfect pore structures and, in the case of salt, require a lengthy process to remove the salt after the pores are created, said Guillermo Ameer, professor of biomedical engineering at the McCormick School of Engineering and professor of surgery at the Feinberg School of Medicine.
The new scaffolds are more flexible and can be tailored to ‘resorb’ at different times,
The new scaffolds, created from a combination of ceramic nanoparticles and elastic polymers, were formed in a vacuum through a process termed “low-pressure foaming” that requires high heat, Ameer said. The result was a series of pores that were highly interconnected and not dependent on the use of salt.
The new process creates scaffolds that are highly flexible and can be tailored to degrade at varying speeds depending on the recovery time expected for the patient. The scaffolds can also incorporate nano-sized fibers, providing a new range of mechanical and biological properties, Ameer said. [emphasis mine]
I wonder what “new range of mechanical and biological properties” will be enabled; I was not able to find any speculation.
In the meantime, here’s an image of the scaffolding from the McCormick School (at Northwestern University) http://www.mccormick.northwestern.edu/news/articles/article_1043.html,
For anyone who’s interested in an update on Andemariam Teklesenbet Beyene, according to this Dec. 9, 2011 posting on StemSave, he’s doing well.
ETA Feb. 14, 2012: Michael Berger at Nanowerk has written an article titled, Tissue engineering of 3D tubular structures, which provides some insight into another aspect of creating scaffolding, the tubular nature of many of our organs.