It seems chimeras are of more interest these days. In all likelihood that has something to do with the fellow who received a transplant of a pig’s heart in January 2022 (he died in March 2022).
For those who aren’t familiar with the term, a chimera is an entity with two different DNA (deoxyribonucleic acid) identities. In short, if you get a DNA sample from the heart, it’s different from a DNA sample obtained from a cheek swab. This contrasts with a hybrid such as a mule (donkey/horse) whose DNA samples show a consisted identity throughout its body.
A December 12, 2022 The Hastings Center news release (also on EurekAlert) announces a special report,
A new report on the ethics of crossing species boundaries by inserting human cells into nonhuman animals – research surrounded by debate – makes recommendations clarifying the ethical issues and calling for improved oversight of this work.
The report, “Creating Chimeric Animals — Seeking Clarity On Ethics and Oversight,” was developed by an interdisciplinary team, with funding from the National Institutes of Health. Principal investigators are Josephine Johnston and Karen Maschke, research scholars at The Hastings Center, and Insoo Hyun, director of the Center for Life Sciences and Public Learning at the Museum of Life Sciences in Boston, formerly of Case Western Reserve University.
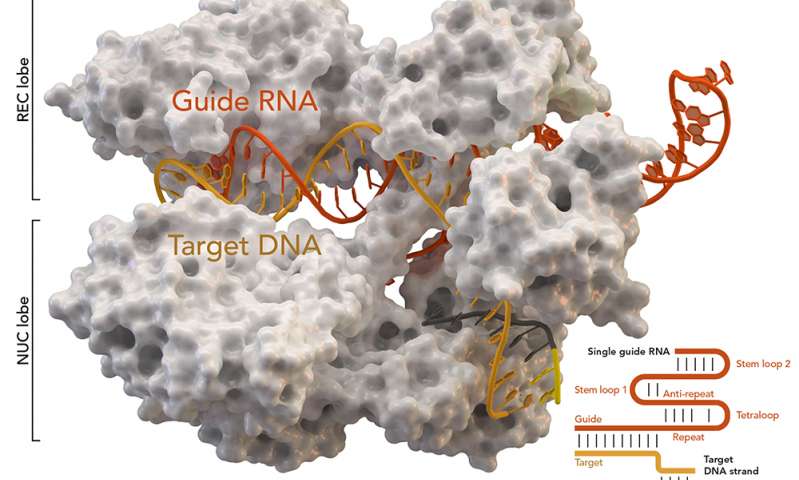
Advances in human stem cell science and gene editing enable scientists to insert human cells more extensively and precisely into nonhuman animals, creating “chimeric” animals, embryos, and other organisms that contain a mix of human and nonhuman cells.
Many people hope that this research will yield enormous benefits, including better models of human disease, inexpensive sources of human eggs and embryos for research, and sources of tissues and organs suitable for transplantation into humans.
But there are ethical concerns about this type of research, which raise questions such as whether the moral status of nonhuman animals is altered by the insertion of human stem cells, whether these studies should be subject to additional prohibitions or oversight, and whether this kind of research should be done at all.
The report found that:
Animal welfare is a primary ethical issue and should be a focus of ethical and policy analysis as well as the governance and oversight of chimeric research.
Chimeric studies raise the possibility of unique or novel harms resulting from the insertion and development of human stem cells in nonhuman animals, particularly when those cells develop in the brain or central nervous system.
Oversight and governance of chimeric research are siloed, and public communication is minimal. Public communication should be improved, communication between the different committees involved in oversight at each institution should be enhanced, and a national mechanism created for those involved in oversight of these studies.
Scientists, journalists, bioethicists, and others writing about chimeric research should use precise and accessible language that clarifies rather than obscures the ethical issues at stake. The terms “chimera,” which in Greek mythology refers to a fire-breathing monster, and “humanization” are examples of ethically laden, or overly broad language to be avoided.
The Research Team
The Hastings Center
• Josephine Johnston
• Karen J. Maschke
• Carolyn P. Neuhaus
• Margaret M. Matthews
• Isabel BoloCase Western Reserve University
• Insoo Hyun (now at Museum of Science, Boston)
• Patricia Marshall
• Kaitlynn P. CraigThe Work Group
• Kara Drolet, Oregon Health & Science University
• Henry T. Greely, Stanford University
• Lori R. Hill, MD Anderson Cancer Center
• Amy Hinterberger, King’s College London
• Elisa A. Hurley, Public Responsibility in Medicine and Research
• Robert Kesterson, University of Alabama at Birmingham
• Jonathan Kimmelman, McGill University
• Nancy M. P. King, Wake Forest University School of Medicine
• Geoffrey Lomax, California Institute for Regenerative Medicine
• Melissa J. Lopes, Harvard University Embryonic Stem Cell Research Oversight Committee
• P. Pearl O’Rourke, Harvard Medical School
• Brendan Parent, NYU Grossman School of Medicine
• Steven Peckman, University of California, Los Angeles
• Monika Piotrowska, State University of New York at Albany
• May Schwarz, The Salk Institute for Biological Studies
• Jeff Sebo, New York University
• Chris Stodgell, University of Rochester
• Robert Streiffer, University of Wisconsin-Madison
• Lorenz Studer, Memorial Sloan Kettering Cancer Center
• Amy Wilkerson, The Rockefeller University
Here’s a link to and a citation for the report,
Creating Chimeric Animals: Seeking Clarity on Ethics and Oversight edited by Karen J. Maschke, Margaret M. Matthews, Kaitlynn P. Craig, Carolyn P. Neuhaus, Insoo Hyun, Josephine Johnston, The Hastings Center Report Volume 52, Issue S2 (Special Report), November‐December 2022 First Published: 09 December 2022
This report is open access.