I’ve not actively kept up with the situation in the West African countries suffering an outbreak of the ebola virus other than to note that it is ongoing. My Aug. 15, 2014 post provides a snapshot of the situation and various new treatments, including one based on tobacco, which could be helpful but appeared not to have been tested and/or deployed. There was a lot of secrecy (especially from Medicago, a Canadian company) regarding the whole matter of treatments and vaccines.
There seem to have been some new developments on the treatment side, involving yet another Canadian company, Tekmira, according to a Sept. 23, 2013 news item on Azonano,
Tekmira Pharmaceuticals Corporation, a leading developer of RNA interference (RNAi) therapeutics, today announced that the FDA [US Food and Drug Administration] has authorized Tekmira to provide TKM-Ebola for treatment under expanded access protocols to subjects with confirmed or suspected Ebola virus infections.
A Sept. 22, 2014 Tekmira news release, which originated the news item, expands on the topic of regulatory issues associated with bringing this treatment to the areas suffering the outbreak,
“Tekmira is reporting that an appropriate regulatory and clinical framework is now in place to allow the use of TKM-Ebola in patients. We have worked with the FDA and Health Canada to establish this framework and a treatment protocol allowing us to do what we can to help these patients,” said Dr. Mark J. Murray Tekmira’s President and CEO.
“We have insisted on acting responsibly in the interest of patients and our stakeholders,” added Dr. Murray. “Today we are reporting that, working closely with regulators in the United States and Canada, we have established a framework for TKM-Ebola use in multiple patients. In the US, the FDA has granted expanded access use of TKM-Ebola under our Investigational New Drug application (IND) and Health Canada has established a similar framework, both of which allow the use of our investigational therapeutic in more patients.”
“We have already responded to requests for the use of our investigational agent in several patients under emergency protocols, in an effort to help these patients, a goal we share with the FDA and Health Canada. TKM-Ebola has been administered to a number of patients and the repeat infusions have been well tolerated. However, it must be kept in mind that any uses of the product under expanded access, does not constitute controlled clinical trials. These patients may be infected with a strain of Ebola virus which has emerged subsequent to the strain that our product is directed against, and physicians treating these patients may use more than one therapeutic intervention in an effort to achieve the best outcome,” said Dr. Murray. “Our TKM-Ebola drug supplies are limited, but we will continue to help where we can, as we continue to focus on the other important objectives we have to advance therapies to meet the unmet needs of patients.”
TKM-Ebola is an investigational therapeutic, being developed under an FDA approved IND, which is currently the subject of a partial clinical hold under which the FDA has allowed the potential use of TKM-Ebola in individuals with a confirmed or suspected Ebola virus infection.
About FDA Expanded Access Program
Expanded access is the use of an investigational drug outside of a clinical trial to treat a patient, with a serious or immediately life-threatening disease or condition, who has no comparable or satisfactory alternative treatment options. FDA regulations allow access to investigational drugs for treatment purposes on a case-by-case basis for an individual patient, or for intermediate-size groups of patients with similar treatment needs who otherwise do not qualify to participate in a clinical trial. (Source: www.fda.com)
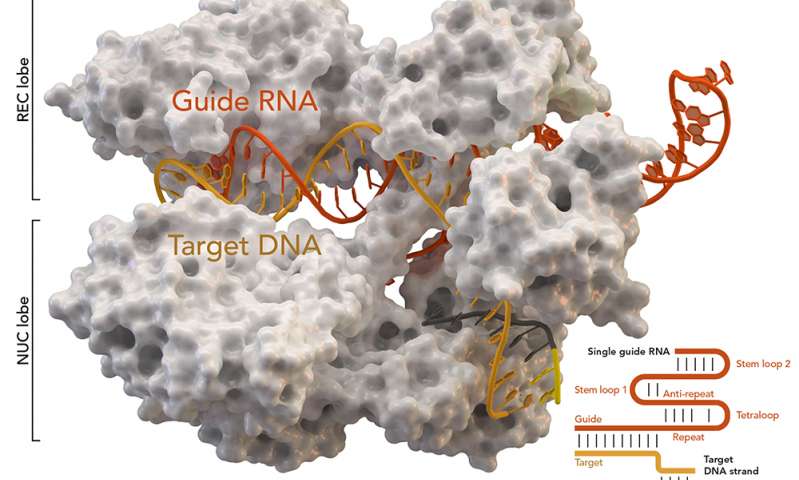
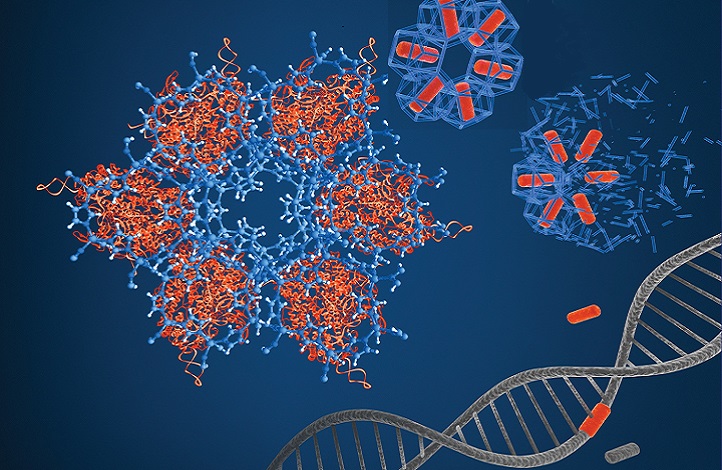
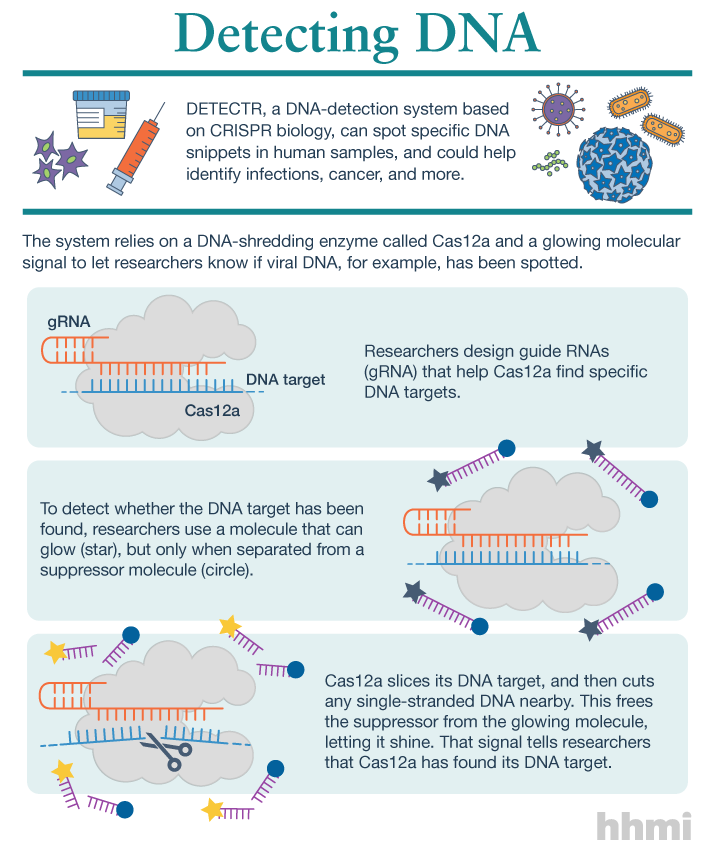
About TKM-Ebola, an Anti-Ebola Virus RNAi Therapeutic
TKM-Ebola, an anti-Ebola virus RNAi therapeutic, is being developed under a $140 million contract with the U.S. Department of Defense’s Medical Countermeasure Systems BioDefense Therapeutics (MCS-BDTX) Joint Product Management Office. Earlier preclinical studies were published in the medical journal The Lancet and demonstrated that when siRNA targeting the Ebola virus and delivered by Tekmira’s LNP [Lipid Nanoparticle] technology were used to treat previously infected non-human primates, the result was 100 percent protection from an otherwise lethal dose of Zaire Ebola virus (Geisbert et al., The Lancet, Vol. 375, May 29, 2010). In March 2014, Tekmira was granted a Fast Track designation from the U.S. Food and Drug Administration for the development of TKM-Ebola.
About Joint Project Manager Medical Countermeasure Systems (JPM-MCS)
This work is being conducted under contract with the U.S. Department of Defense Joint Project Manager Medical Countermeasure Systems (JPM-MCS). JPM-MCS, a component of the Joint Program Executive Office for Chemical and Biological Defense, aims to provide U.S. military forces and the nation with safe, effective, and innovative medical solutions to counter chemical, biological, radiological, and nuclear threats. JPM-MCS facilitates the advanced development and acquisition of medical countermeasures and systems to enhance biodefense response capability. For more information, visit www.jpeocbd.osd.mil.
About Tekmira
Tekmira Pharmaceuticals Corporation is a biopharmaceutical company focused on advancing novel RNAi therapeutics and providing its leading lipid nanoparticle (LNP) delivery technology to pharmaceutical partners. Tekmira has been working in the field of nucleic acid delivery for over a decade and has broad intellectual property covering LNPs. Further information about Tekmira can be found at www.tekmira.com. Tekmira is based in Vancouver, B.C. Canada.
Forward-Looking Statements and Information
This news release contains “forward-looking statements” or “forward-looking information” within the meaning of applicable securities laws (collectively, “forward-looking statements”). Forward-looking statements in this news release include statements about Tekmira’s strategy, future operations, clinical trials, prospects and the plans of management; an appropriate regulatory and clinical framework for emergency use of TKM-Ebola in subjects with confirmed or suspected Ebola infections; FDA grant of expanded access use of TKM-Ebola under Tekmira’s IND; Health Canada’s establishment of a similar framework for TKM-Ebola; Tekmira’s response to requests for the use of TKM-Ebola in several patients under emergency protocols and the results thereon; the current supply of TKM-Ebola drug; the partial clinical hold on the TKM-Ebola IND by the FDA (enabling the potential use of TKM-Ebola in individuals with a confirmed or suspected Ebola virus infection); the quantum value of the contract with the JPM-MCS; and Fast Track designation from the FDA for the development of TKM-Ebola.
With respect to the forward-looking statements contained in this news release, Tekmira has made numerous assumptions regarding, among other things, the clinical framework for emergency use of TKM-Ebola. While Tekmira considers these assumptions to be reasonable, these assumptions are inherently subject to significant business, economic, competitive, market and social uncertainties and contingencies.
Additionally, there are known and unknown risk factors which could cause Tekmira’s actual results, performance or achievements to be materially different from any future results, performance or achievements expressed or implied by the forward-looking statements contained herein. Known risk factors include, among others: TKM-Ebola may not prove to be effective in the treatment of Ebola infection under the emergency use framework, or at all; any uses of TKM-Ebola under emergency INDs are not controlled trails, and TKM-Ebola may be used on Ebola strains that have diverged from the strain to which TKM-Ebola is directed, and physicians treating patients may use more than one therapeutic intervention in addition to TKM-Ebola; the current supply of TKM-Ebola is limited, and Tekmira may not be able to respond to future requests for help in the current Ebola outbreak; the FDA may not remove the partial clinical hold on the TKM-Ebola IND; the FDA may refuse to approve Tekmira’s products, or place restrictions on Tekmira’s ability to commercialize its products; anticipated pre-clinical and clinical trials may be more costly or take longer to complete than anticipated, and may never be initiated or completed, or may not generate results that warrant future development of the tested drug candidate; and Tekmira may not receive the necessary regulatory approvals for the clinical development of Tekmira’s products.
A more complete discussion of the risks and uncertainties facing Tekmira appears in Tekmira’s Annual Report on Form 10-K and Tekmira’s continuous disclosure filings, which are available at www.sedar.com or www.sec.gov. All forward-looking statements herein are qualified in their entirety by this cautionary statement, and Tekmira disclaims any obligation to revise or update any such forward-looking statements or to publicly announce the result of any revisions to any of the forward-looking statements contained herein to reflect future results, events or developments, except as required by law.
In the midst of all those ‘cover your rear end’ statements to investors, it’s easy to miss the fact that people are actually being treated and the results are promising, if not guaranteed,
Tekmira has distributed a Sept. 23, 2014 news release touting its membership in a new consortium, which suggests that in parallel with offering treatment, human clinical trials will also be conducted,
Tekmira Pharmaceuticals Corporation (Nasdaq:TKMR) (TSX:TKM), a leading developer of RNA interference (RNAi) therapeutics, today reported that it is collaborating with an international consortium to provide an RNAi based investigational therapeutic for expedited clinical studies in West Africa.
Led by Dr. Peter Horby of the Centre for Tropical Medicine and Global Health at the University of Oxford and the International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC), the consortium includes representatives from the World Health Organization (WHO), US Centers for Disease Control, Médecins Sans Frontières – Doctors without Borders (MSF), ISARIC, and Fondation Mérieux, among others.
The Wellcome Trust has announced it has awarded £3.2 million to the consortium to fund this initiative. The award will include funds for the manufacture of investigational therapeutics as well as the establishment of an operational clinical trials platform in two or more Ebola Virus Disease (EVD) treatment centers in West Africa. RNAi has been prioritized as an investigational therapeutic and may be selected for clinical trials at these centers.
The objective of the clinical trials is to assess the efficacy and safety of promising therapeutics and vaccines, reliably and safely, in patients with EVD by adopting strict protocols that comply with international standards. It is hoped this initiative will permit the adoption of safe and effective interventions rapidly.
The genetic sequence of the Ebola virus variant responsible for the ongoing outbreak in West Africa is now available. Under this program, Tekmira will produce an RNAi based product specifically targeting the viral variant responsible for this outbreak. The ability to rapidly and accurately match the evolving genetic sequences of emerging infectious agents is one of the powerful features of RNAi therapeutics.
“We commend the Wellcome Trust for their leadership in providing the necessary funds to launch and expedite this ground breaking initiative. We are gratified that RNAi has been prioritized as a potential investigational therapeutic to assist in the ongoing public health and humanitarian crisis in Africa,” said Dr. Murray, Tekmira’s President and CEO.
“We are an active collaborator in this consortium and through our ongoing dialogue with the WHO, NGOs and governments in various countries; we have been discussing the creation of appropriate clinical and regulatory frameworks for the potential use of investigational therapeutics in Africa. This initiative goes a long way towards achieving this aim. Many complex decisions remain to fully implement this unique clinical trial platform. At this time, there can be no assurances that our product will be selected by the consortium for clinical trials in Africa,” said Dr. Murray.
About Wellcome Trust
The Wellcome Trust is the largest charity in the UK. It funds innovative biomedical research, in the UK and internationally, spending over £600 million each year to support the brightest scientists with the best ideas. The Wellcome Trust supports public debate about biomedical research and its impact on health and wellbeing. For more information, visit www.wellcome.ac.uk
I’m glad they’re being careful while giving people treatment, i. e., trying to do something rather than waiting to conduct human clinical trials as has sometimes been the case in the past. This business of running the trials almost parallel to offering treatment suggests an agility not often associated with the international health care community.
ETA Sept. 23 2014 1200 hours PDT: For more information about the status of the Ebola outbreak read Tara Smith’s Sept. 22, 2014 article Slate titled, Here’s Where We Stand With Ebola; Even experienced international disaster responders are shocked at how bad it’s gotten (Note: Links have been removed).
Now, terms like “exponential spread” are being thrown around as the epidemic continues to expand more and more rapidly. Just last week, an increase of 700 new cases was reported, and the case count is now doubling in size approximately every three weeks.
…
A Doctors Without Borders worker in Monrovia, Liberia, named Jackson Naimah describes the situation in his home country, noting that patients are literally dying at the front door of his treatment center because it lacks patient beds and assistance; the sufferers are left to die a “horrible, undignified death” and potentially infect others as they do so: …
…
… Health care workers who are treating the sick are dying because they also lack basic protective equipment, or because they have been so overwhelmed by taking care of the ill and dying that they begin to make potentially fatal errors. They have gone on strike in Liberia because they are not being adequately protected or even paid for their risky service.
…
Fear and misinformation are as deadly as the virus itself. Eight Ebola workers were recently murdered in Guinea, in the area where the virus first came to the world’s attention in March. Liberia’s largest newspaper featured a story describing Ebola as a man-made virus being purposely unleashed upon Africans by Western pharmaceutical companies. Reports abound of doctors and other workers being chased away, sometimes violently, by fearful families. …
It’s not a pleasant read but, I think, a necessary one. For anyone who may think the panic and fear are unique to this situation, I once worked with a nurse who described being lifted by her neck after someone came through the door of a clinic demanding a vaccine and had been refused. He was in such a panic and so fearful he wasn’t going to take a ‘no’. The incident took place in Vancouver (Canada) in a ‘nice’ part of town.
ETA Sept. 24, 2014: Kelly Grant has written a Sept. 22, 2014 article for the Globe and Mail which provides more information about Tekmira, some of which contradicts the details I have here about TKM-Ebola and clinical trials in Africa although the key points remain the same. She also provides more information about the ZMapp therapy (mentioned in my Aug. 15, 2014 post) noting yet a third Canadian connection.* Canada’s National Microbiology Laboratory was somehow involved in developing ZMApp, unfortunately, Grant does not or is not able to provide more details about that involvement.
ETA Oct. 16, 2014: David Bruggeman recommends a digital journalism site Ebola Deeply for some in depth reporting in his Oct. 16, 2014 posting.
* This sentence “She also provides more information about the ZMapp therapy mentioned in my Aug. 15, 2014 post mentioning yet a third Canadian connection.” was altered for grammatical purposes on Dec. 4, 2014.