There are three ‘eye’-related items in this piece, two of them concerning animal eyes and one concerning a camera-eye or the possibility of superhuman sight.
Earlier this week researchers at the University of Reading (UK) announced they have achieved a better understanding of how nanoparticles might be able to bypass some of the eye’s natural barriers in the hopes of making eye drops more effective in an Oct. 7, 2014 news item on Nanowerk,
Sufferers of eye disorders have new hope after researchers at the University of Reading discovered a potential way of making eye drops more effective.
Typically less than 5% of the medicine dose applied as drops actually penetrates the eye – the majority of the dose will be washed off the cornea by tear fluid and lost.
The team, led by Professor Vitaliy Khutoryanskiy, has developed novel nanoparticles that could attach to the cornea and resist the wash out effect for an extended period of time. If these nanoparticles are loaded with a drug, their longer attachment to the cornea will ensure more medicine penetrates the eye and improves drop treatment.
An Oct. 6, 2014 University of Reading press release, which originated the news item, provides more information about the hoped for impact of this work while providing few details about the research (Note: A link has been removed),
The research could also pave the way for new treatments of currently incurable eye-disorders such as Age-related Macular Degeneration (AMD) – the leading cause of visual impairment with around 500,000 sufferers in the UK.
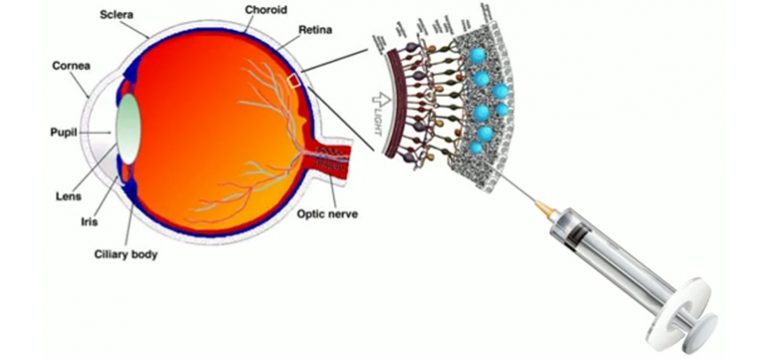
There is currently no cure for this condition but experts believe the progression of AMD could be slowed considerably using injections of medicines into the eye. However, eye-drops with drug-loaded nanoparticles could be a potentially more effective and desirable course of treatment.
Professor Vitaliy Khutoryanskiy, from the University of Reading’s School of Pharmacy, said: “Treating eye disorders is a challenging task. Our corneas allow us to see and serve as a barrier that protects our eyes from microbial and chemical intervention. Unfortunately this barrier hinders the effectiveness of eye drops. Many medicines administered to the eye are inefficient as they often cannot penetrate the cornea barrier. Only the very small molecules in eye drops can penetrate healthy cornea.
“Many recent breakthroughs to treat eye conditions involve the use of drugs incorporated into nano-containers; their role being to promote drug penetration into the eye. However the factors affecting this penetration remain poorly understood. Our research also showed that penetration of small drug molecules could be improved by adding enhancers such as cyclodextrins. This means eye drops have the potential to be a more effective, and a more comfortable, future treatment for disorders such as AMD.”
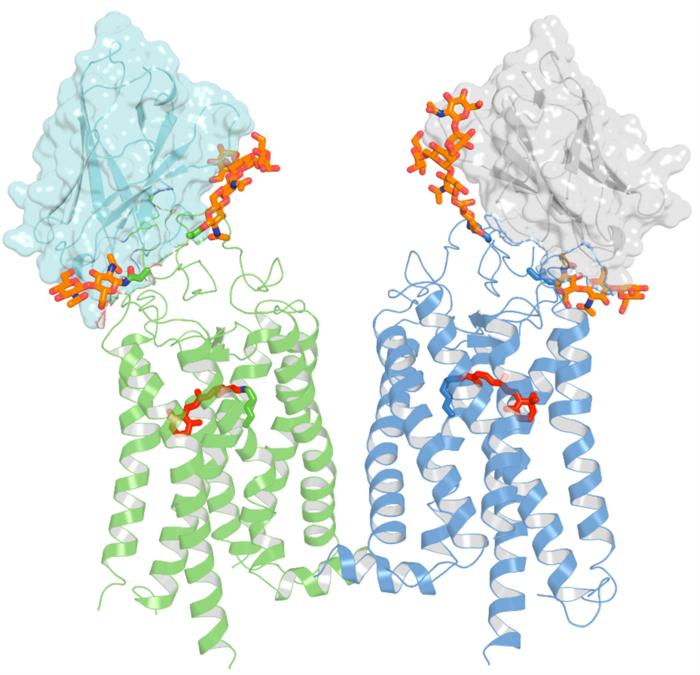
The finding is one of a number of important discoveries highlighted in a paper published today in the journal Molecular Pharmaceutics. The researchers revealed fascinating insights into how the structure of the cornea prevents various small and large molecules, as well as nanoparticles, from entering into the eye. They also examined the effects any damage to the eye would have in allowing these materials to enter the body.
Professor Khutoryanskiy continued: “There is increasing concern about the safety of environmental contaminants, pollutants and nanoparticles and their potential impacts on human health. We tested nanoparticles whose sizes ranged between 21 – 69 nm, similar to the size of viruses such as polio, or similar to airborn particles originating from building industry and found that they could not penetrate healthy and intact cornea irrespective of their chemical nature.
“However if the top layer of the cornea is damaged, either after surgical operation or accidentally, then the eye’s natural defence may be compromised and it becomes susceptible to viral attack which could result in eye infections.
“The results show that our eyes are well-equipped to defend us against potential airborne threats that exist in a fast-developing industrialised world. However we need to be aware of the potential complications that may arise if the cornea is damaged, and not treated quickly and effectively.”
Here’s a link to and a citation for the paper,
On the Barrier Properties of the Cornea: A Microscopy Study of the Penetration of Fluorescently Labeled Nanoparticles, Polymers, and Sodium Fluorescein by Ellina A. Mun, Peter W. J. Morrison, Adrian C. Williams, and Vitaliy V. Khutoryanskiy. Mol. Pharmaceutics, 2014, 11 (10), pp 3556–3564 DOI: 10.1021/mp500332m Publication Date (Web): August 28, 2014
Copyright © 2014 American Chemical Society
There’s a little more information to be had in the paper’s abstract, which is, as these things go, is relatively accessible,
![[downloaded from http://pubs.acs.org/doi/abs/10.1021/mp500332m]](http://www.frogheart.ca/wp-content/uploads/2014/10/eye-300x154.gif)
[downloaded from http://pubs.acs.org/doi/abs/10.1021/mp500332m]
The paper is behind a paywall. No mention is made in the abstract or in the press release as to how the bovine (ox, cow, or buffalo) eyes were obtained but I gather these body parts are often harvested from animals that have been previously slaughtered for food.
This next item also concerns research about eye drops but this time the work comes from the University of Waterloo (Ontario, Canada). From an Oct. 8, 2014 news item on Azonano,
For the millions of sufferers of dry eye syndrome, their only recourse to easing the painful condition is to use drug-laced eye drops three times a day. Now, researchers from the University of Waterloo have developed a topical solution containing nanoparticles that will combat dry eye syndrome with only one application a week.
An Oct. 8, 2014 University of Waterloo news release (also on EurekAlert), which originated the news item, describes the results of the work without providing much detail about the nanoparticles used to deliver the treatment via eye drops,
The eye drops progressively deliver the right amount of drug-infused nanoparticles to the surface of the eyeball over a period of five days before the body absorbs them. One weekly dose replaces 15 or more to treat the pain and irritation of dry eyes.
The nanoparticles, about 1/1000th the width of a human hair, stick harmlessly to the eye’s surface and use only five per cent of the drug normally required.
“You can’t tell the difference between these nanoparticle eye drops and water,” said Shengyan (Sandy) Liu, a PhD candidate at Waterloo’s Faculty of Engineering, who led the team of researchers from the Department of Chemical Engineering and the Centre for Contact Lens Research. “There’s no irritation to the eye.”
Dry eye syndrome is a more common ailment for people over the age of 50 and may eventually lead to eye damage. More than six per cent of people in the U.S. have it. Currently, patients must frequently apply the medicine three times a day because of the eye’s ability to self-cleanse—a process that washes away 95 per cent of the drug.
“I knew that if we focused on infusing biocompatible nanoparticles with Cyclosporine A, the drug in the eye drops, and make them stick to the eyeball without irritation for longer periods of time, it would also save patients time and reduce the possibility of toxic exposure due to excessive use of eye drops,” said Liu.
The research team is now focusing on preparing the nanoparticle eye drops for clinical trials with the hope that this nanoparticle therapy could reach the shelves of drugstores within five years.
Here’s a link to and a citation for the paper,
Phenylboronic acid modified mucoadhesive nanoparticle drug carriers facilitate weekly treatment of experimentallyinduced dry eye syndrome by Shengyan Liu, Chu Ning Chang, Mohit S. Verma, Denise Hileeto, Alex Muntz, Ulrike Stahl, Jill Woods, Lyndon W. Jones, and Frank X. Gu. Nano Research (October 2014) DOI: 10.1007/s12274-014-0547-3
This paper is behind a paywall. There is a partial preview available for free. As per the paper’s abstract, research was performed on healthy rabbit eyes.
The last ‘sight’ item I’m featuring here comes from the Massachusetts Institute of Technology (MIT) and does not appear to have been occasioned by the publication of a research paper or some other event. From an Oct. 7, 2014 news item on Azonano,
All through his childhood, Ramesh Raskar wished fervently for eyes in the back of his head. “I had the notion that the world did not exist if I wasn’t looking at it, so I would constantly turn around to see if it was there behind me.” Although this head-spinning habit faded during his teen years, Raskar never lost the desire to possess the widest possible field of vision.
Today, as director of the Camera Culture research group and associate professor of Media Arts and Sciences at the MIT Media Lab, Raskar is realizing his childhood fantasy, and then some. His inventions include a nanocamera that operates at the speed of light and do-it-yourself tools for medical imaging. His scientific mission? “I want to create not just a new kind of vision, but superhuman vision,” Raskar says.
An Oct. 6, 2014 MIT news release, which originated the news item, provides more information about Raskar and his research,
He avoids research projects launched with a goal in mind, “because then you only come up with the same solutions as everyone else.” Discoveries tend to cascade from one area into another. For instance, Raskar’s novel computational methods for reducing motion blur in photography suggested new techniques for analyzing how light propagates. “We do matchmaking; what we do here can be used over there,” says Raskar.
Inspired by the famous microflash photograph of a bullet piercing an apple, created in 1964 by MIT professor and inventor Harold “Doc” Edgerton, Raskar realized, “I can do Edgerton millions of times faster.” This led to one of the Camera Culture group’s breakthrough inventions, femtophotography, a process for recording light in flight.
Manipulating photons into a packet resembling Edgerton’s bullet, Raskar and his team were able to “shoot” ultrashort laser pulses through a Coke bottle. Using a special camera to capture the action of these pulses at half a trillion frames per second with two-trillionths of a second exposure times, they captured moving images of light, complete with wave-like shadows lapping at the exterior of the bottle.
Femtophotography opened up additional avenues of inquiry, as Raskar pondered what other features of the world superfast imaging processes might reveal. He was particularly intrigued by scattered light, the kind in evidence when fog creates the visual equivalent of “noise.”
In one experiment, Raskar’s team concealed an object behind a wall, out of camera view. By firing super-short laser bursts onto a surface nearby, and taking millions of exposures of light bouncing like a pinball around the scene, the group rendered a picture of the hidden object. They had effectively created a camera that peers around corners, an invention that might someday help emergency responders safely investigate a dangerous environment.
Raskar’s objective of “making the invisible visible” extends as well to the human body. The Camera Culture group has developed a technique for taking pictures of the eye using cellphone attachments, spawning inexpensive, patient-managed vision and disease diagnostics. Conventional photography has evolved from time-consuming film development to instantaneous digital snaps, and Raskar believes “the same thing will happen to medical imaging.” His research group intends “to break all the rules and be at the forefront. I think we’ll get there in the next few years,” he says.
Ultimately, Raskar predicts, imaging will serve as a catalyst of transformation in all dimensions of human life — change that can’t come soon enough for him. “I hate ordinary cameras,” he says. “They record only what I see. I want a camera that gives me a superhuman perspective.”
Following the link to the MIT news release will lead you to more information about Raskar and his work. You can also see and hear Raskar talk about his femtophotography in a 2012 TEDGlobal talk here.



![[downloaded from http://pubs.acs.org/doi/abs/10.1021/mp500332m]](http://www.frogheart.ca/wp-content/uploads/2014/10/eye-300x154.gif)