I imagine that most anyone who’s been in contact with Ms. Shoichet is experiencing a thrill on hearing this morning’s (November 10, 2020) news about winning Canada’s highest honour for science and engineering research. (Confession: she, very kindly, once gave me a brief interview for a posting on this blog, more about that later).
Why Molly Shoichet won the Gerhard Herzberg Canada Gold Medal
Emily Chung’s Nov. 10, 2020 news item on the Canadian Broadcasting Corporation (CBC) website announces the exciting news (Note: Links have been removed),
A Toronto chemical engineering professor has won the $1 million Gerhard Herzberg Canada Gold Medal, the country’s top science prize, for her work designing gels that mimic human tissues.
The Natural Sciences and Engineering Research Council of Canada (NSERC) announced Tuesday [Nov. 10, 2020] that Molly Shoichet, professor of chemical engineering and applied chemistry and Canada Research Chair in Tissue Engineering at the University of Toronto is this year’s recipient of the award, which recognizes “sustained excellence” and “overall influence” of research conducted in Canada in the natural sciences or engineering.
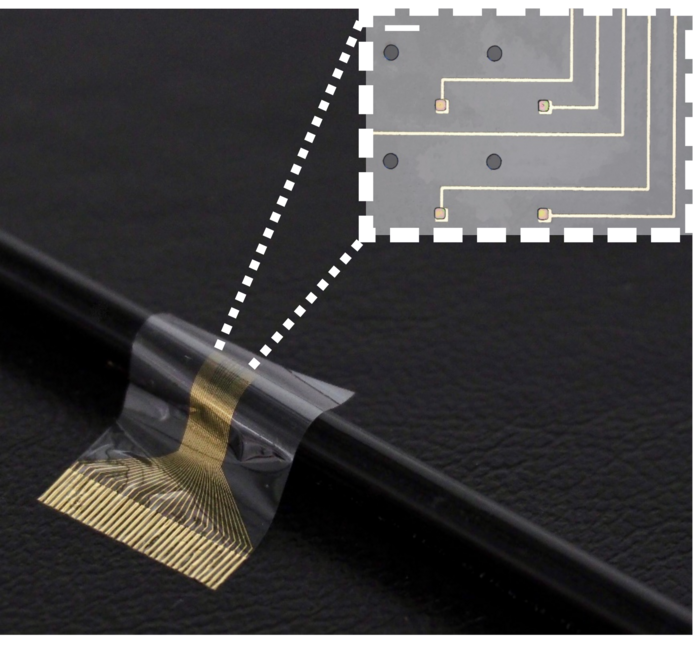
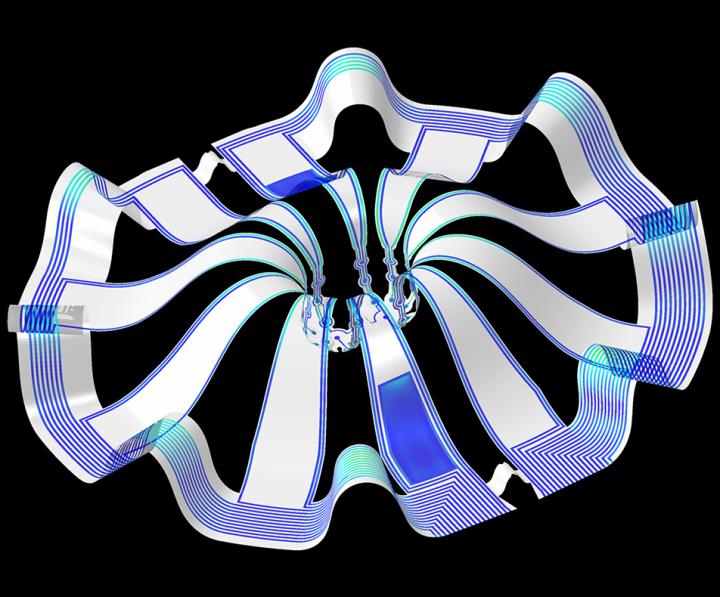
Shoichet’s hydrogels are used for drug development and delivery and regenerative medicine to heal injuries and treat diseases.
…
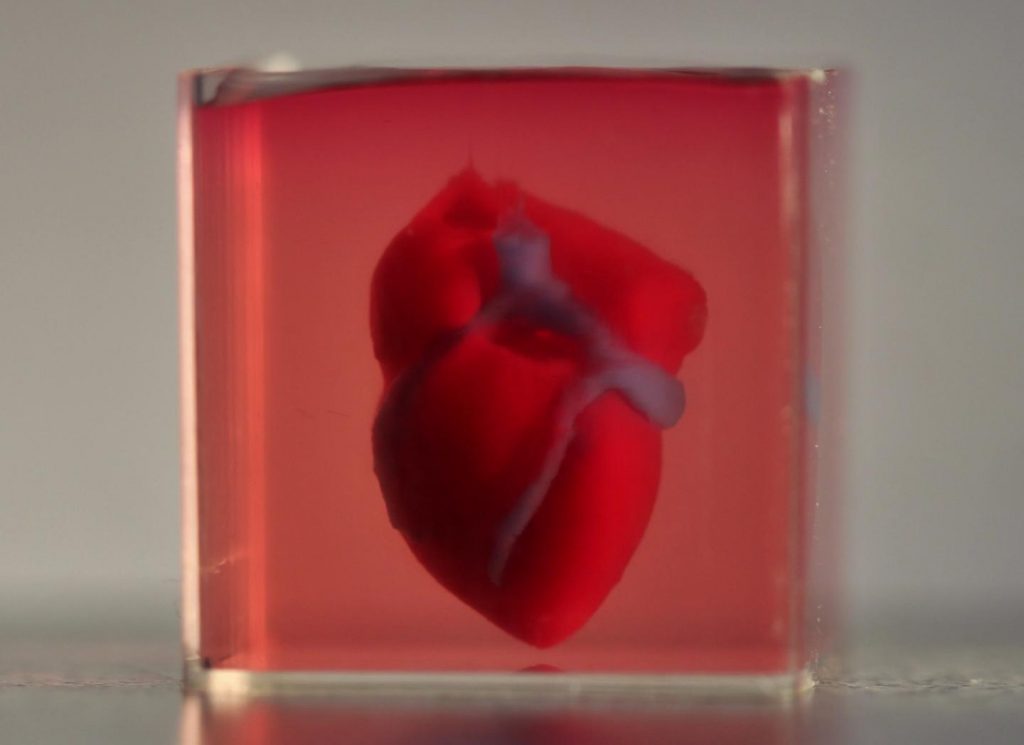
NSERC said Shoichet’s work has led to the development of several “game-changing” applications of such materials. They “delivered a crucial breakthrough” by allowing cells to be grown in three dimensions as they do in the body, rather than the two dimensions they typically do in a petri dish.
…
Hydrogels are polymer materials — materials such as plastics, made of repeating units — that become swollen with water.
“If you’ve ever eaten Jell-o, that’s a hydrogel,” Shoichet said. Slime and the absorbent material inside disposable diapers are also hydrogels.
…
Shoichet was born in Toronto, and studied science and engineering at the Massachusetts Institute of Technology and the University of Massachusetts Amherst. After graduating, she worked in the biotech industry alongside “brilliant biologists,” she said. She noticed that the biologists’ research was limited by what types of materials were available.
As an engineer, she realized she could help by custom designing materials for biologists. She could make materials specifically suit their needs, to answer their specific questions by designing hydrogels to mimic particular tissues.
…
Her collaborations with biologists have also generated three spinoff companies, including AmacaThera, which was recently approved to run human trials of a long-acting anesthetic delivered with an injectable hydrogel to deal with post-surgical pain.
Shoichet noted that drugs given to deal with that kind of pain lead to a quarter of opioid addictions, which have been a deadly problem in Canada and around the world.
“What we’re really excited about is not only meeting that critical need of providing people with greater pain relief for a sustained period of time, but also possibly putting a dent in the operation,” she said.
…
Liz Do’s Nov. 10, 2020 University of Toronto news release provides more details (Note: Links have been removed),
…
The Herzberg Gold Medal is awarded by the Natural Sciences and Engineering Research Council (NSERC) in recognition of research contributions characterized by both excellence and influence.
“I was completely overwhelmed when I was told the good news,” says Shoichet. “There are so many exceptional people who’ve won this award and I admire them. To think of my peers putting me in that same category is really incredible.”
A pioneer in regenerative medicine, tissue engineering and drug delivery, Shoichet and her team are internationally known for their discovery and innovative use of 3D hydrogels.
“One of the challenges facing drug screening is that many of the drugs discovered work well in the lab, but not in people, and a possible explanation for this discrepancy is that these drugs are discovered in environments that do not reflect that of the body,” explains Shoichet.
Shoichet’s team has invented a series of biomaterials that provide a soft, three-dimensional environment in which to grow cells. These hydrogels — water-swollen materials — better mimic human tissue than hard two-dimensional plastic dishes that are typically used. “Now we can do more predictive drug screening,” says Shoichet.
Her lab is using these biomaterials to discover drugs for breast and brain cancer and a rare lung disease. Shoichet’s lab has been equally innovative in regenerative medicine strategies to promote repair of the brain after stroke and overcome blindness.
“Everything that we do is motivated by answering a question in biology, using our engineering and chemistry tools to answer those questions,” says Shoichet.
“The hope is that our contributions will ultimately make a positive impact in the cancer community and in treating diseases for which we can only slow the progression rather than stop and reverse, such as with blindness.”
Shoichet is also an advocate for and advisor on the fields of science and engineering. She has advised both federal and provincial governments through her service on Canada’s Science, Technology and Innovation Council and the Ontario Research Innovation Council. From 2014 to 2018, she was the Senior Advisor to the President on Science & Engineering Engagement at the University of Toronto. She is the co-founder of Research2Reality [emphasis mine], which uses social media to promote innovative research across the country. She also served as Ontario’s first Chief Scientist [emphasis mine], with a mandate to advance science and innovation in the province.
Shoichet is the only person to be elected a fellow of all three of Canada’s National Academies and is a foreign member of the U.S. National Academy of Engineering, and fellow of the Royal Society (UK) — the oldest and most prestigious academic society.
…
Doug Ford (premier of Ontario) and Molly Shoichet
She did serve as Ontario’s first Chief Scientist—for about six months (Nov. 2017 – July 2018). Molly Shoichet was fired when a new provincial government was elected in the summer of 2018. Here’s more about the incident from a July 4, 2018 article by Ryan Maloney for huffingtonpost.ca (Note: Links have been removed),
New Ontario Premier Doug Ford has fired the province’s first chief scientist.
Dr. Molly Shoichet, a renowned biomedical engineer who teaches at the University of Toronto, was appointed in November [2017] to advise the government and ensure science and research were at the forefront of decision-making.
Shoichet told HuffPost Canada in an email that the she does not believe the decision was about her, and “I don’t even know whether it was about this role.” She said she is disappointed but honoured to have served Ontarians, even for a short time.
Ford’s spokesman, Simon Jefferies told The Canadian Press Wednesday that the government is starting the process of “finding a suitable and qualified replacement.” [emphasis mine]
The move comes just days after Ford’s Progressive Conservatives officially took power in Canada’s largest province with a majority government.
…
Almost a year later, there was no replacement in sight according to a June 24, 2019 opinion piece by Kimberly Girling (then the Research and Policy Director of the Evidence for Democracy not-for-profit) for the star.com,
Premier Doug Ford, I’m concerned for your government.
I know you feel it too. Last week, one year into your mandate and faced with sharply declining polls after your first provincial budget, you conducted a major cabinet shuffle. This shuffle is clearly an attempt to “put the right people in the right place at the right time” and improve the outcomes of your cabinet. But I’m still concerned.
Since your election, your caucus has made many bold decisions. Unfortunately, it seems many are Ontarians unhappy with most of these decisions, and I’m not sure the current shuffle is enough to fix this.
…
[] I think you’re missing someone.
What about a Chief Scientist?
It isn’t a radical idea. Actually, you used to have one. Ontario’s first Chief Scientist, Dr. Molly Shoichet, was appointed to advise the government on science policy and champion science and innovation for Ontario. However, when your government was elected, you fired Dr. Shoichet within the first week.
It’s been a year, and so far we haven’t seen any attempts to fill this vacant position. [emphasis mine]
…
I wonder if Doug Ford and his crew regret the decision to fire Shoichet especially now that the province is suffering from a new peak in rising COVID-19 case numbers. These days government could do with a little bit of good news.
The only way we might ever know is if Doug Ford writes a memoir (in about 20 or 30 years from now).
Molly Shoichet, Research2Reality, and FrogHeart
A May 11, 2015 posting announced the launch of Research2Reality and it’s in this posting that I have a few comments from Molly Shoichet about co-founding a national science communication project. Given how busy she was at the time, I was amazed she took a few minutes to speak to me and took more time to make it possible for me to interview Raymond Laflamme (then director of the Institute for Quantum Computing at the University of Waterloo [Ontario]) and a prominent physicist.
Here are the comments Molly Shoichet offered (from the May 11, 2015 posting),
…
“I’m very excited about this and really hope that other people will be too,” says Shoichet. The audience for the Research2Reality endeavour is for people who like to know more and have questions when they see news items about science discoveries that can’t be answered by investigating mainstream media programmes or trying to read complex research papers.
This is a big undertaking. ” Mike [Mike MacMillan, co-founder] and I thought about this for about two years.” Building on the support they received from the University of Toronto, “We reached out to the vice-presidents of research at the top fifteen universities in the country.” In the end, six universities accepted the invitation to invest in this project,
…
Five years later, it’s still going.
Finally: Congratulations Molly Shoichet!