A November 14, 2017 news item on phys.org announces a grant for a research project which will see engineered robot hands combined with regenerative medicine to imbue neuroprosthetic hands with the sense of touch,
The sense of touch is often taken for granted. For someone without a limb or hand, losing that sense of touch can be devastating. While highly sophisticated prostheses with complex moving fingers and joints are available to mimic almost every hand motion, they remain frustratingly difficult and unnatural for the user. This is largely because they lack the tactile experience that guides every movement. This void in sensation results in limited use or abandonment of these very expensive artificial devices. So why not make a prosthesis that can actually “feel” its environment?
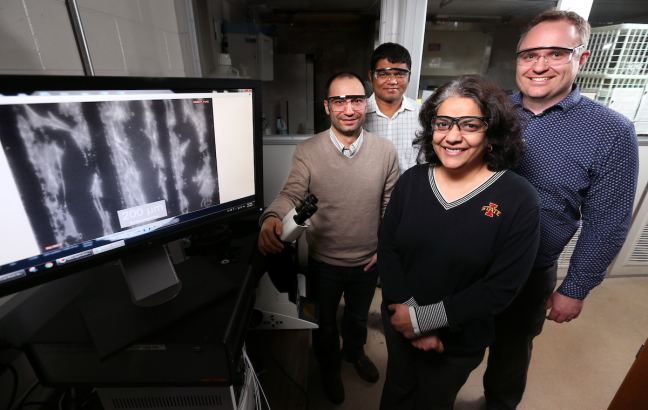
That is exactly what an interdisciplinary team of scientists from Florida Atlantic University and the University of Utah School of Medicine aims to do. They are developing a first-of-its-kind bioengineered robotic hand that will grow and adapt to its environment. This “living” robot will have its own peripheral nervous system directly linking robotic sensors and actuators. FAU’s College of Engineering and Computer Science is leading the multidisciplinary team that has received a four-year, $1.3 million grant from the National Institute of Biomedical Imaging and Bioengineering of the [US] National Institutes of Health for a project titled “Virtual Neuroprosthesis: Restoring Autonomy to People Suffering from Neurotrauma.”
A November14, 2017 Florida Atlantic University (FAU) news release by Gisele Galoustian, which originated the news item, goes into more detail,
With expertise in robotics, bioengineering, behavioral science, nerve regeneration, electrophysiology, microfluidic devices, and orthopedic surgery, the research team is creating a living pathway from the robot’s touch sensation to the user’s brain to help amputees control the robotic hand. A neuroprosthesis platform will enable them to explore how neurons and behavior can work together to regenerate the sensation of touch in an artificial limb.
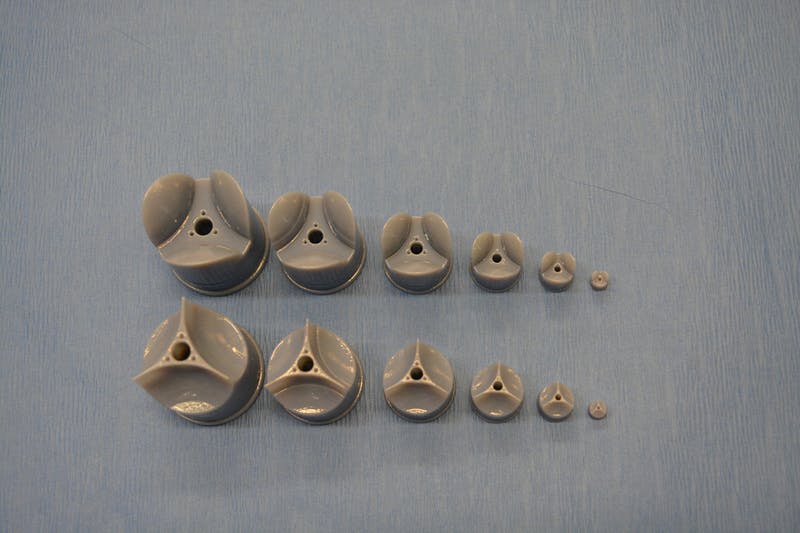
At the core of this project is a cutting-edge robotic hand and arm developed in the BioRobotics Laboratory in FAU’s College of Engineering and Computer Science. Just like human fingertips, the robotic hand is equipped with numerous sensory receptors that respond to changes in the environment. Controlled by a human, it can sense pressure changes, interpret the information it is receiving and interact with various objects. It adjusts its grip based on an object’s weight or fragility. But the real challenge is figuring out how to send that information back to the brain using living residual neural pathways to replace those that have been damaged or destroyed by trauma.
“When the peripheral nerve is cut or damaged, it uses the rich electrical activity that tactile receptors create to restore itself. We want to examine how the fingertip sensors can help damaged or severed nerves regenerate,” said Erik Engeberg, Ph.D., principal investigator, an associate professor in FAU’s Department of Ocean and Mechanical Engineering, and director of FAU’s BioRobotics Laboratory. “To accomplish this, we are going to directly connect these living nerves in vitro and then electrically stimulate them on a daily basis with sensors from the robotic hand to see how the nerves grow and regenerate while the hand is operated by limb-absent people.”
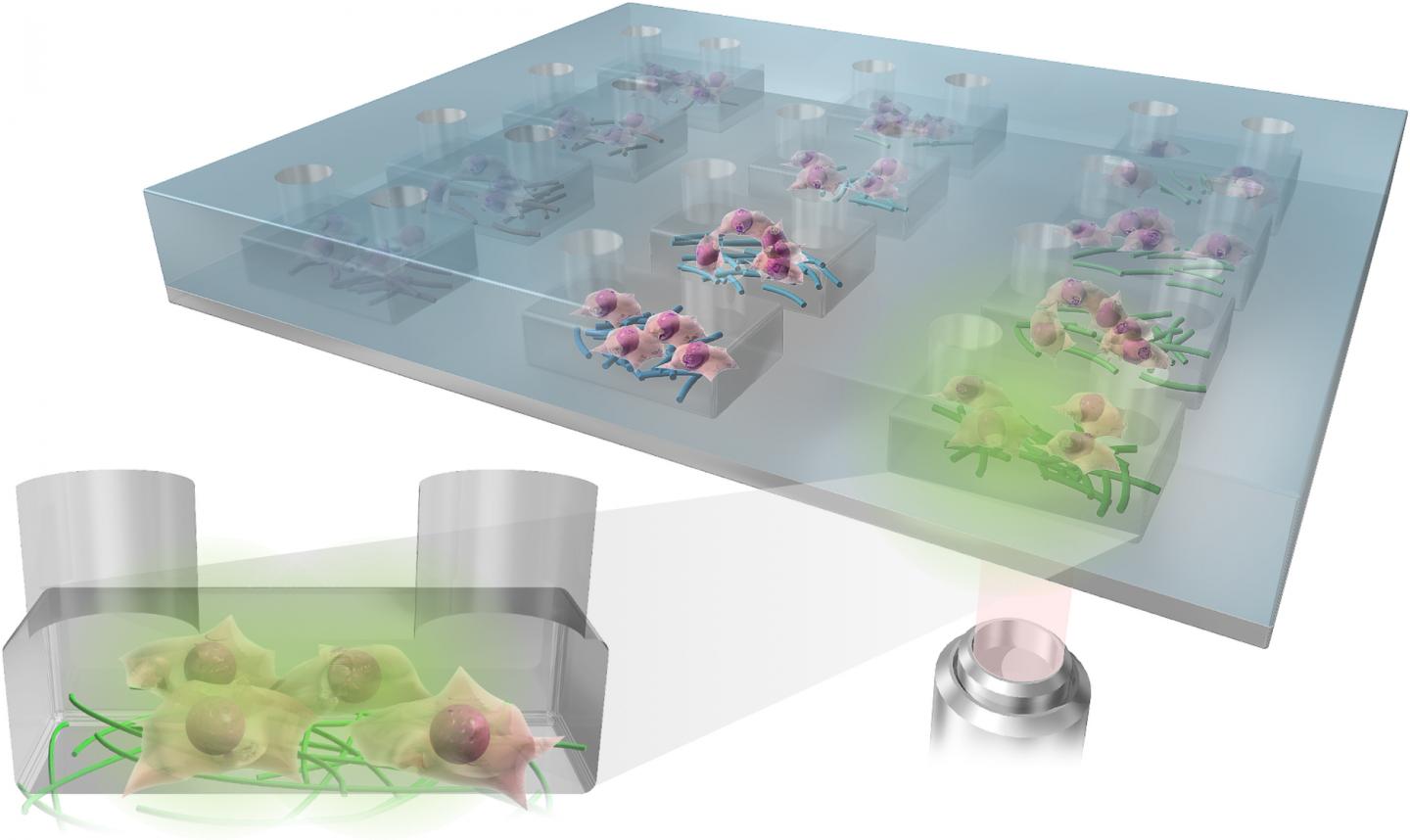
For the study, the neurons will not be kept in conventional petri dishes. Instead, they will be placed in biocompatible microfluidic chambers that provide a nurturing environment mimicking the basic function of living cells. Sarah E. Du, Ph.D., co-principal investigator, an assistant professor in FAU’s Department of Ocean and Mechanical Engineering, and an expert in the emerging field of microfluidics, has developed these tiny customized artificial chambers with embedded micro-electrodes. The research team will be able to stimulate the neurons with electrical impulses from the robot’s hand to help regrowth after injury. They will morphologically and electrically measure in real-time how much neural tissue has been restored.
Jianning Wei, Ph.D., co-principal investigator, an associate professor of biomedical science in FAU’s Charles E. Schmidt College of Medicine, and an expert in neural damage and regeneration, will prepare the neurons in vitro, observe them grow and see how they fare and regenerate in the aftermath of injury. This “virtual” method will give the research team multiple opportunities to test and retest the nerves without any harm to subjects.
Using an electroencephalogram (EEG) to detect electrical activity in the brain, Emmanuelle Tognoli, Ph.D., co-principal investigator, associate research professor in FAU’s Center for Complex Systems and Brain Sciences in the Charles E. Schmidt College of Science, and an expert in electrophysiology and neural, behavioral, and cognitive sciences, will examine how the tactile information from the robotic sensors is passed onto the brain to distinguish scenarios with successful or unsuccessful functional restoration of the sense of touch. Her objective: to understand how behavior helps nerve regeneration and how this nerve regeneration helps the behavior.
Once the nerve impulses from the robot’s tactile sensors have gone through the microfluidic chamber, they are sent back to the human user manipulating the robotic hand. This is done with a special device that converts the signals coming from the microfluidic chambers into a controllable pressure at a cuff placed on the remaining portion of the amputated person’s arm. Users will know if they are squeezing the object too hard or if they are losing their grip.
Engeberg also is working with Douglas T. Hutchinson, M.D., co-principal investigator and a professor in the Department of Orthopedics at the University of Utah School of Medicine, who specializes in hand and orthopedic surgery. They are developing a set of tasks and behavioral neural indicators of performance that will ultimately reveal how to promote a healthy sensation of touch in amputees and limb-absent people using robotic devices. The research team also is seeking a post-doctoral researcher with multi-disciplinary experience to work on this breakthrough project.
Here’s more about the job opportunity from the FAU BioRobotics Laboratory job posting, (I checked on January 30, 2018 and it seems applications are still being accepted.)
Post-doctoral Opportunity
Dated Posted: Oct. 13, 2017
The BioRobotics Lab at Florida Atlantic University (FAU) invites applications for a NIH NIBIB-funded Postdoctoral position to develop a Virtual Neuroprosthesis aimed at providing a sense of touch in amputees and limb-absent people.
Candidates should have a Ph.D. in one of the following degrees: mechanical engineering, electrical engineering, biomedical engineering, bioengineering or related, with interest and/or experience in transdisciplinary work at the intersection of robotic hands, biology, and biomedical systems. Prior experience in the neural field will be considered an advantage, though not a necessity. Underrepresented minorities and women are warmly encouraged to apply.
The postdoctoral researcher will be co-advised across the department of Mechanical Engineering and the Center for Complex Systems & Brain Sciences through an interdisciplinary team whose expertise spans Robotics, Microfluidics, Behavioral and Clinical Neuroscience and Orthopedic Surgery.
The position will be for one year with a possibility of extension based on performance. Salary will be commensurate with experience and qualifications. Review of applications will begin immediately and continue until the position is filled.
The application should include:
- a cover letter with research interests and experiences,
- a CV, and
- names and contact information for three professional references.
Qualified candidates can contact Erik Engeberg, Ph.D., Associate Professor, in the FAU Department of Ocean and Mechanical Engineering at eengeberg@fau.edu. Please reference AcademicKeys.com in your cover letter when applying for or inquiring about this job announcement.
You can find the apply button on this page. Good luck!